Answer: A
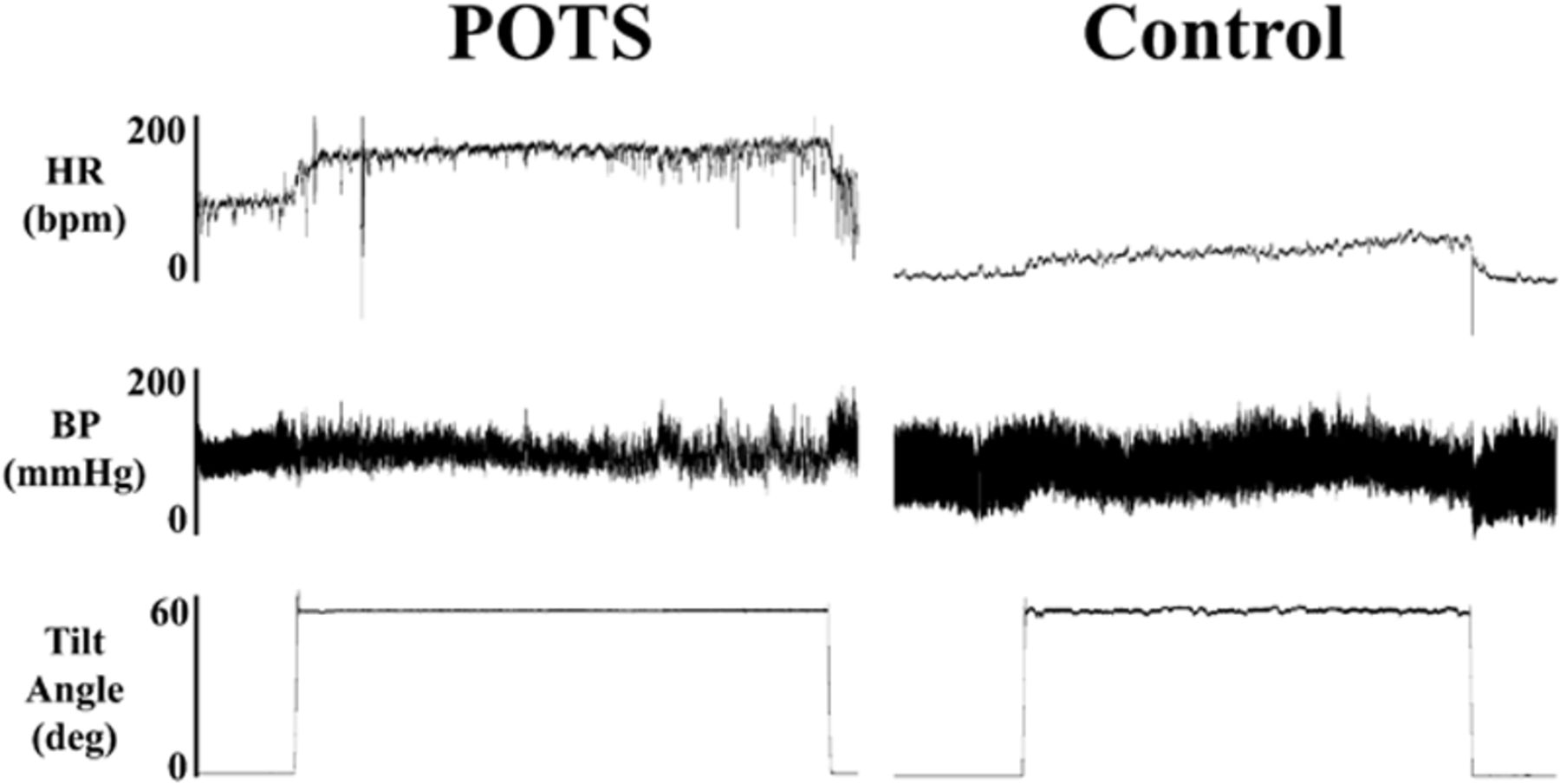
The history and hemodynamics are consistent with postural tachycardia syndrome (POTS),
demonstrating an increase in heart rate when going from sitting to standing.
POTS = orthostatic intolerance in which upright position results in inappropriate tachycardia.
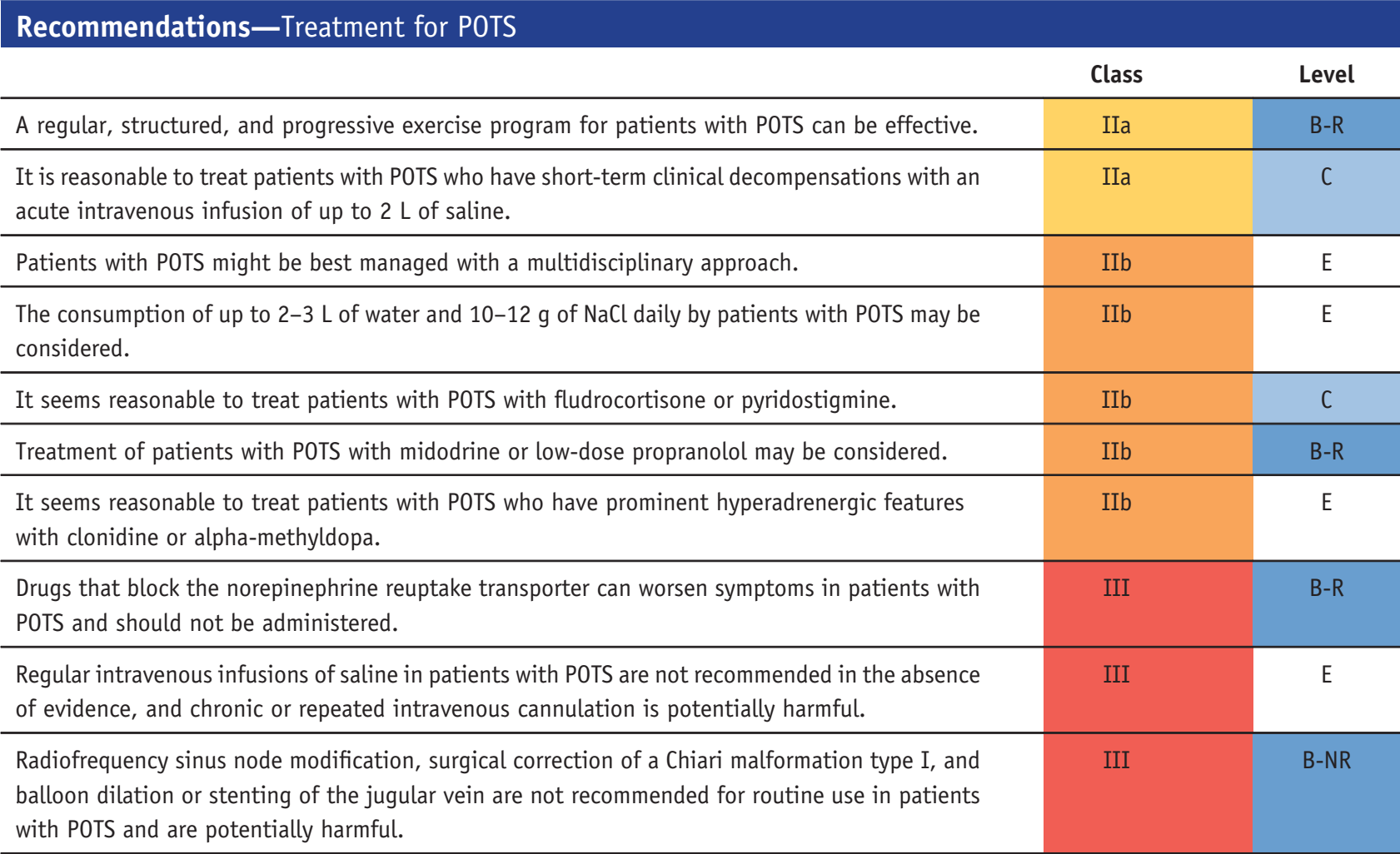
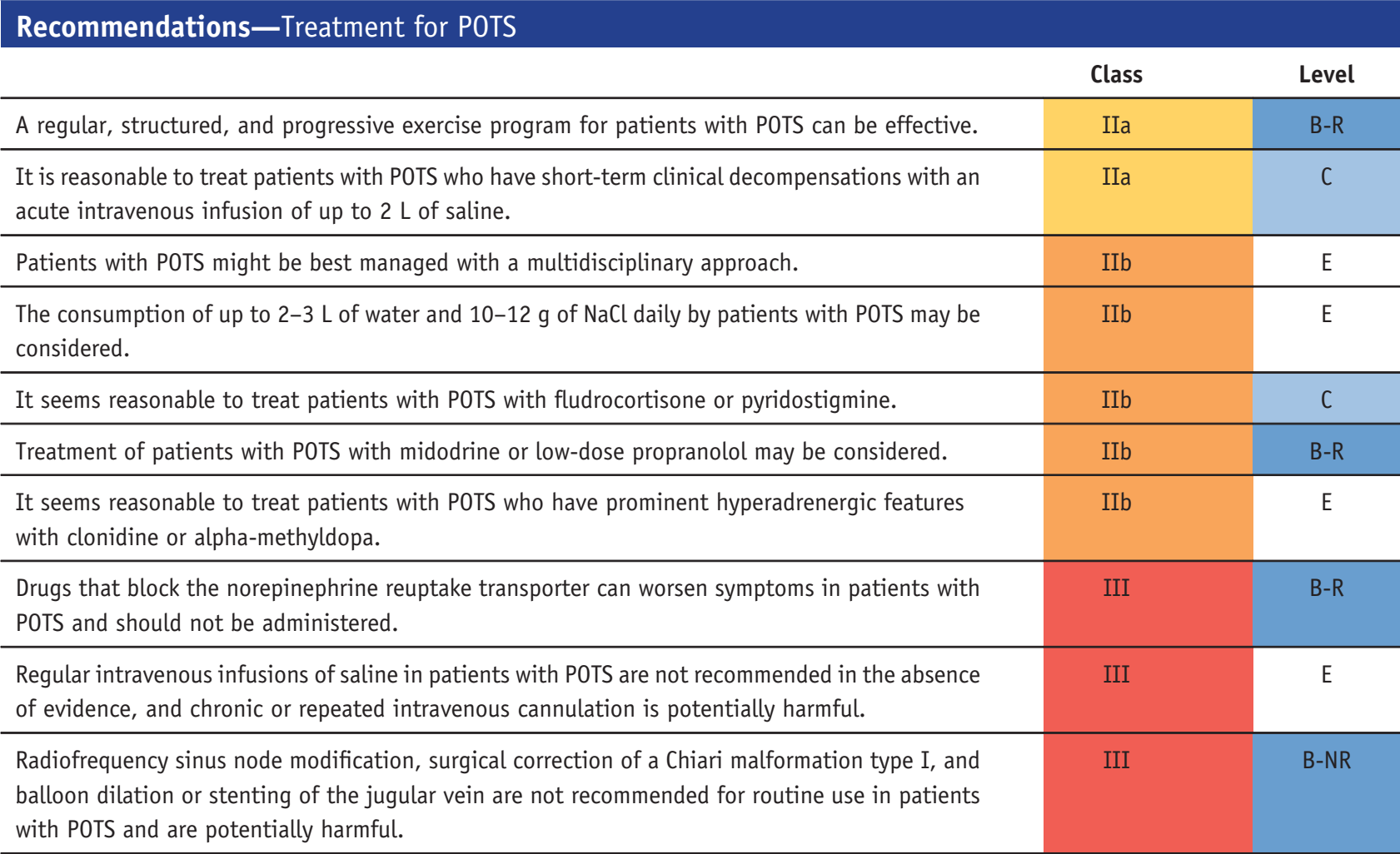
Treatment starts with non-medication first.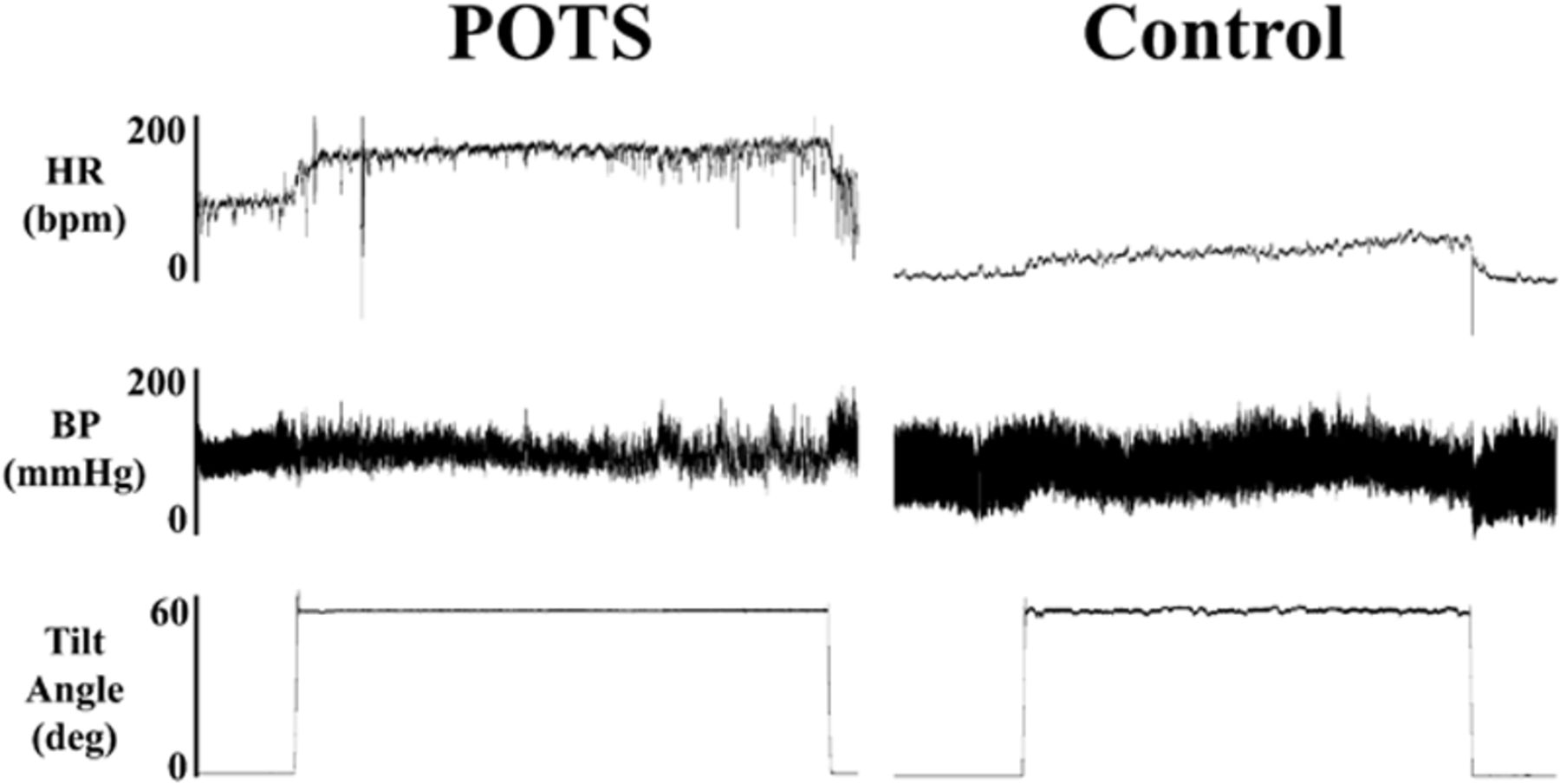
POTS = orthostatic intolerance in which upright position results in inappropriate tachycardia.
Treatment starts with non-medication first.
RELATED
INAPPROPRIATE SINUS TACHYCARDIA
= resting HR>100 and mean 24-hr >90bpm with symptoms, w/o other primary causes.
Ivabradine is recommended as IIa indication.
= resting HR>100 and mean 24-hr >90bpm with symptoms, w/o other primary causes.
Ivabradine is recommended as IIa indication.