A 65-year-old man presents to the emergency department after a syncopal event.
He was eating dinner and was witnessed to abruptly fall back in his chair for
several seconds before regaining consciousness. His past history includes atrial fibrillation
and hypertension. He tells you that 15 years ago, he received a pacemaker
because “his heart stopped.” A generator change was performed 5 years ago.
He has regular pacemaker checks; the last one was 3 months ago, and he was told everything was fine.
His medications include warfarin, metoprolol, and lisinopril.
On examination, his blood pressure is 140/80 mm Hg with a heart rate of 75 bpm.
The physical examination is unremarkable.
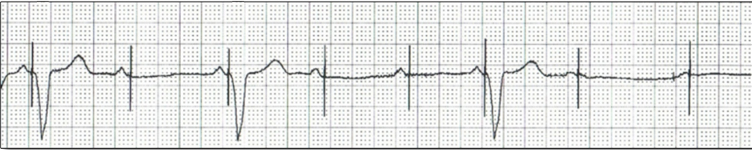
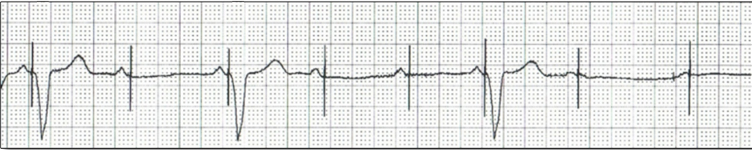
A pacemaker programmer is available to you if needed. As you speak to him, his eyes roll back
and a telemetry strip is recorded (as shown).
Which of the following should be your next step in management of this patient?
- Increase the ventricular sensitivity of the pacemaker.
- Place a magnet over the device.
- Initiate external pacing with cutaneous patches.
- Place a temporary pacemaker.
- Increase the ventricular output of the pacemaker.
Show Answer
Answer: E
Tracing = loss of ventricular capture in an underlying rhythm of complete heart block.
Pacing lead is 15 years old so lead problem is highly possible.
Interrogation will reveal and temporary fix the cause if it is readily available as in this case.
There is no issue of inappropriate sensing so magnet or adjusting sensitivity would not help.