A 63-year-old man has left bundle branch block, a nonischemic cardiomyopathy,
and severe heart failure with NYHA functional class III symptoms despite optimal medical therapy.
He also has had continuous atrial fibrillation for the past seven years,
for which he takes a beta-adrenergic antagonist and digoxin for rate control.
Three months ago, he was referred to you for placement of a CRT-defibrillator.
During the procedure, the left ventricular (LV) lead was placed on the posterolateral wall.
Today, the patient comes to your office for follow-up evaluation. He reports that he feels no better.
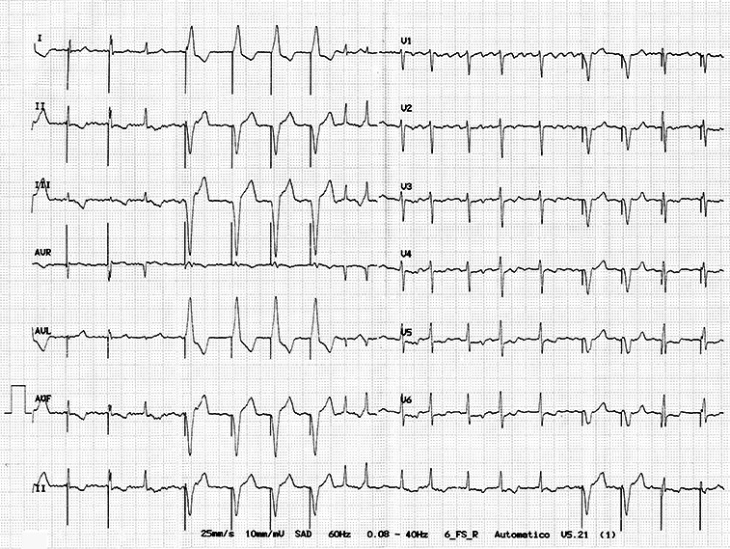
The rhythm strip shown is recorded after device interrogation indicates 94% biventricular pacing.
Which of the following should you do next in order to improve this patient's heart failure?
- Perform cardioversion.
- Perform AV junction ablation.
- Perform speckle-tracking echocardiography in preparation for LV lead revision.
- Reposition the LV lead.
Show Answer
Answer: B
Tracing = AF with BiV pacing with caption, fusion,
and pseudofusion beats.
The patient does not receive 100% BiV pacing due to the presence of AF.
So he is less likely to have improvement in his HF status despite the optimal lead position
and medications for rate control.
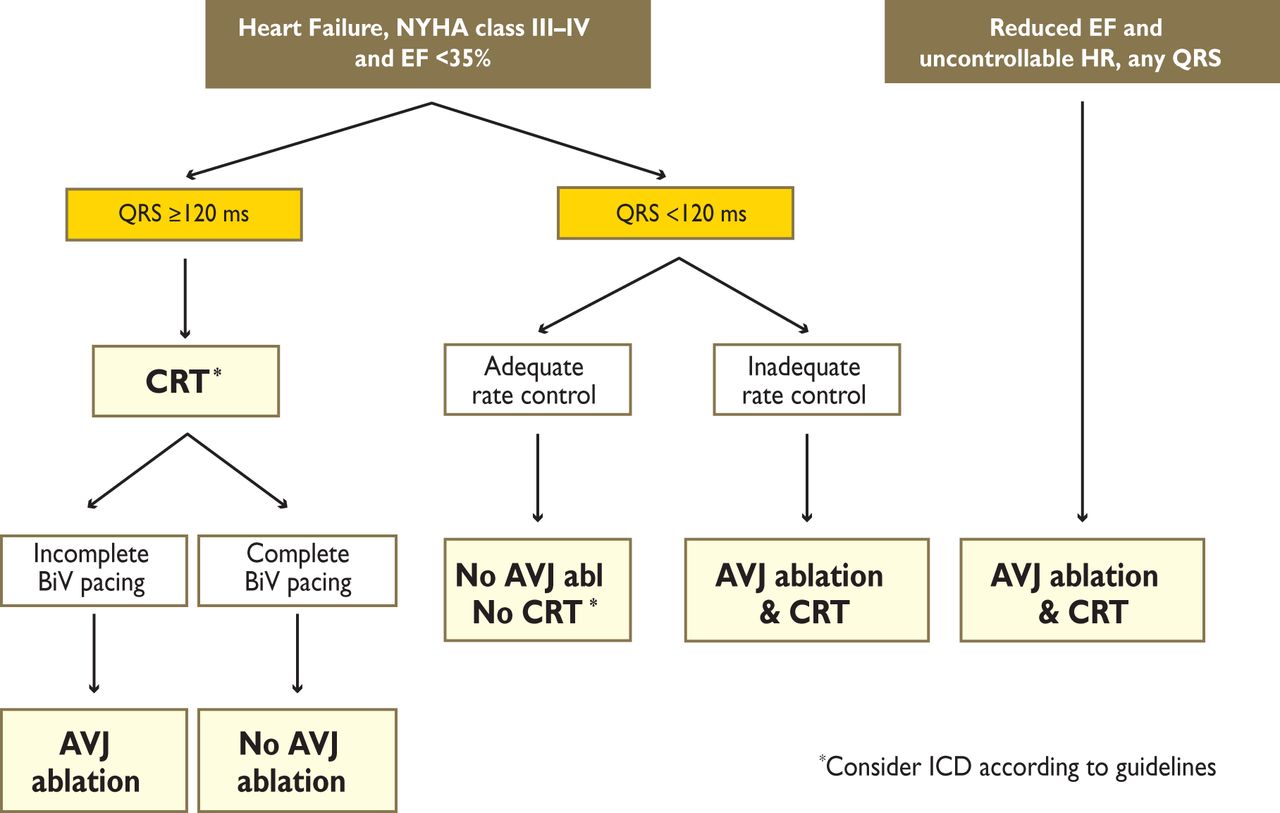
According to
2013 ESC guidelines
, AV nodal ablation should be added (IIa) in case of
incomplete BiV pacing (= not as close to 100%).
Here is the diagram from the guidelines showing indication for
atrioventricular junction (AVJ) ablation in patients with symptomatic
permanent atrial fibrillation (AF) and optimal pharmacological therapy