An 82-year-old Caucasian male with ischemic cardiomyopathy, left ventricular ejection
fraction (LVEF) 0.10, with impaired right ventricular function, patent left internal
mammary artery (LIMA) to the left anterior descending artery (LAD), but multiple occluded
saphenous venous grafts, status/post single lead ICD without history of shocks,
intraventricular conduction delay on electrocardiogram (ECG), heart rate of 66 bpm
off beta-blockers, progressive renal impairment, and three hospitalizations over the prior
calendar year is re-hospitalized and placed on dobutamine for several days. His device is
interrogated and noted to be nearing end-of-life (within 1-3 months). The patient and family
express an interest in proceeding with less aggressive care.
At this juncture, which of the following is the best approach to management of the ICD?
- Selective inactivation of shock therapies while maintaining back-up ventricular pacing.
- Elective generator change.
- Upgrade to a CRT-D.
- Electrophysiological study to evaluate for placement of an atrial lead.
- Use of a beta-blocker with intrinsic sympathomimetic activity.
show answer
Answer: a.
End-of-life care
The decision to inactivate the shock function of a defibrillator needs to take into
account patient preferences and overall prognosis, especially when heart failure symptoms
have progressed despite optimal medical therapy. ACC/AHA guidelines suggest that a reasonable
prognosis for survival of at least 1 year applies to de novo implants; the same applies to
generator changes. Similarly, there are no randomized clinical trials that support CRT upgrades
with this degree of heart failure, though case series have been published.
There is no role for atrial pacing at this juncture; the patient clearly has diffuse conduction
disease and the natural history will not be impacted. There are no data to support the use of any
beta-blocker with intrinsic sympathomimetic activity for any stage of heart failure.
 Our Collection
Our Collection
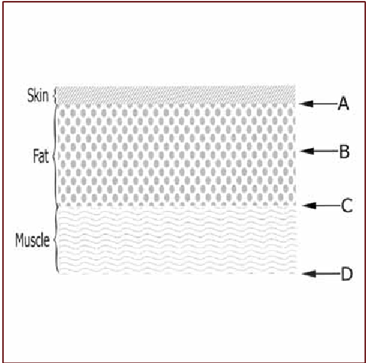
 Principles of Aseptic Technique in an Operating Room
Principles of Aseptic Technique in an Operating Room
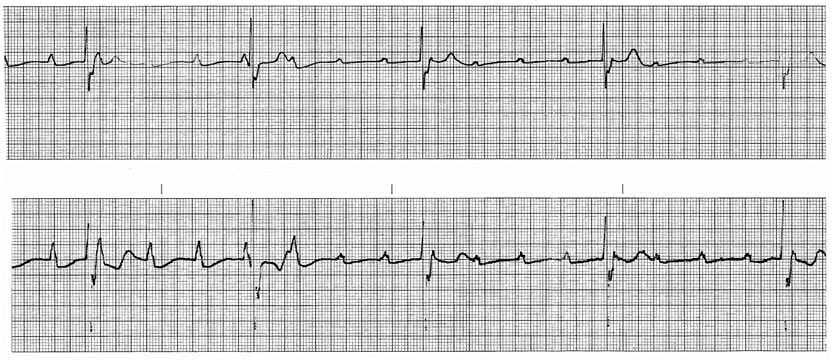
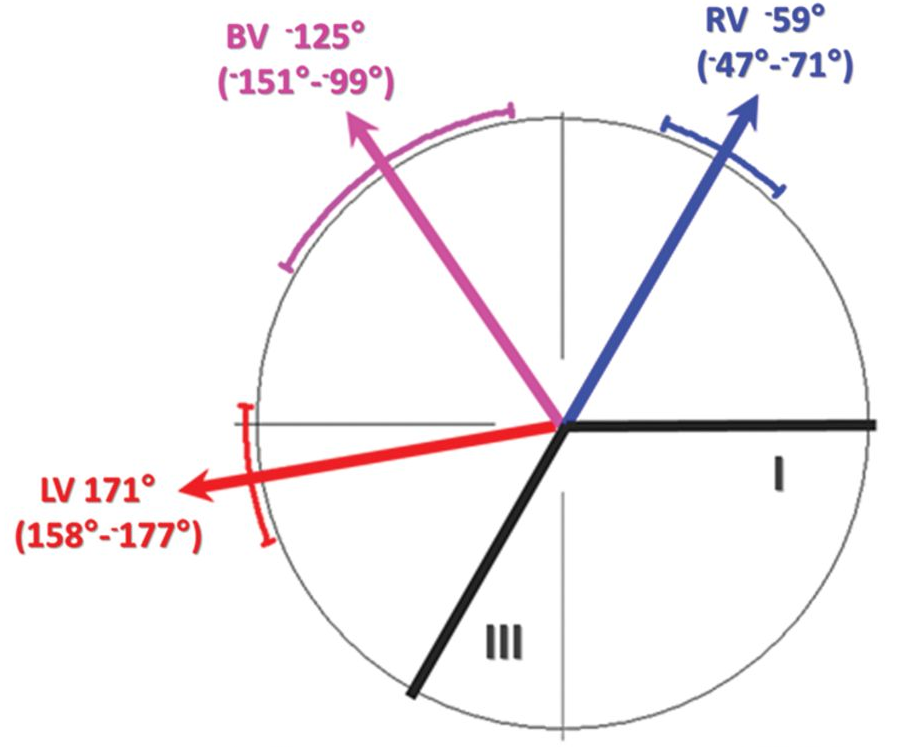
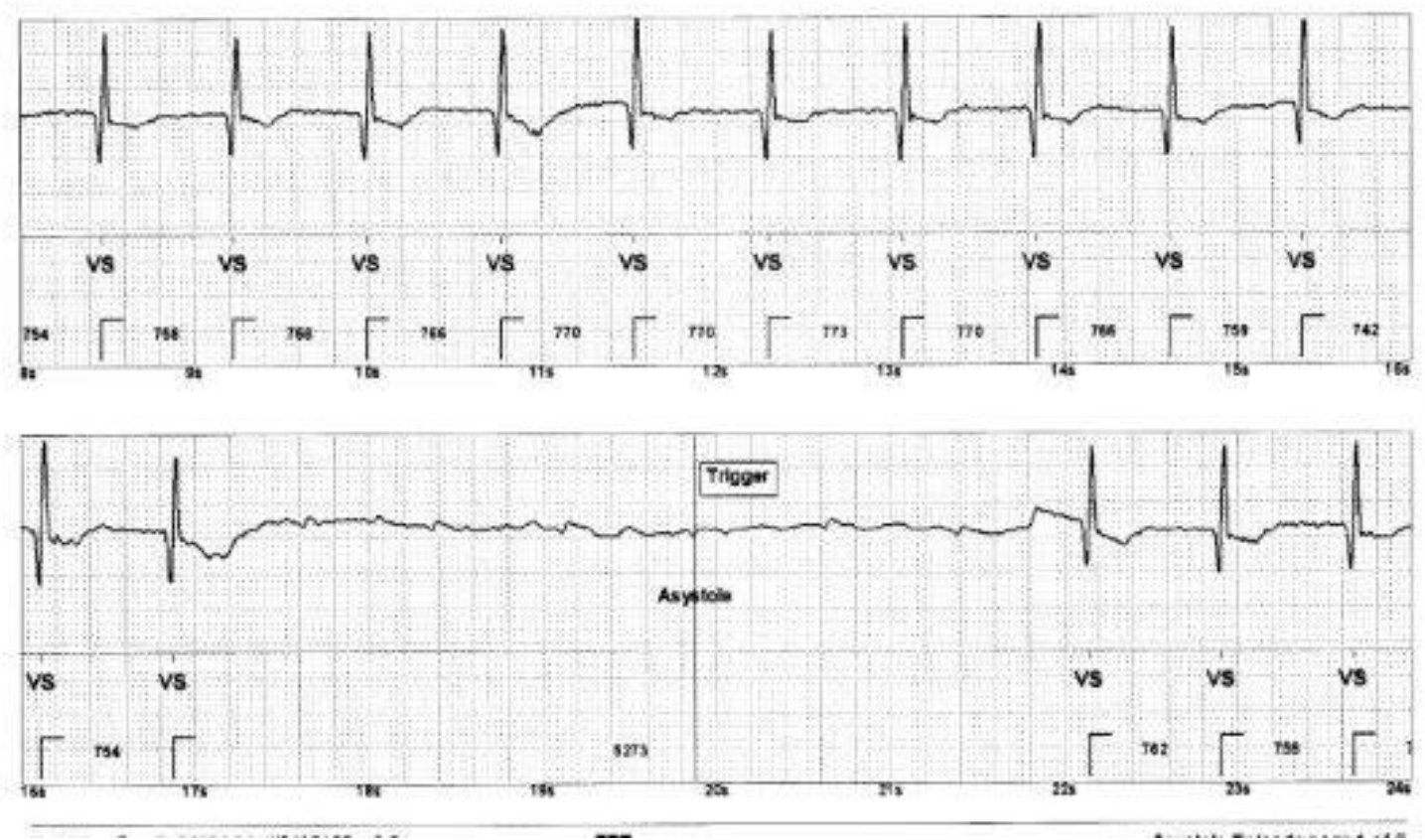
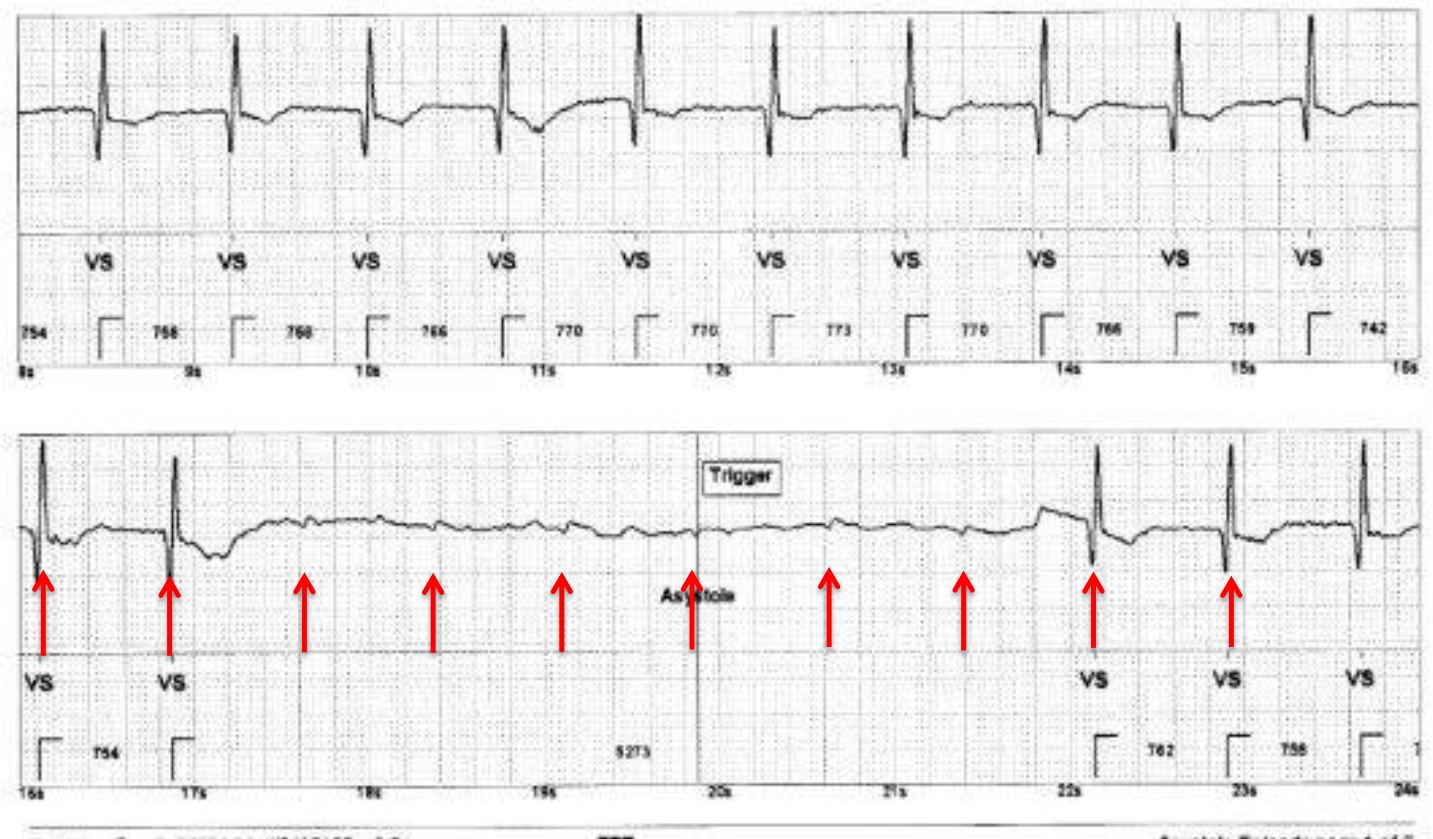
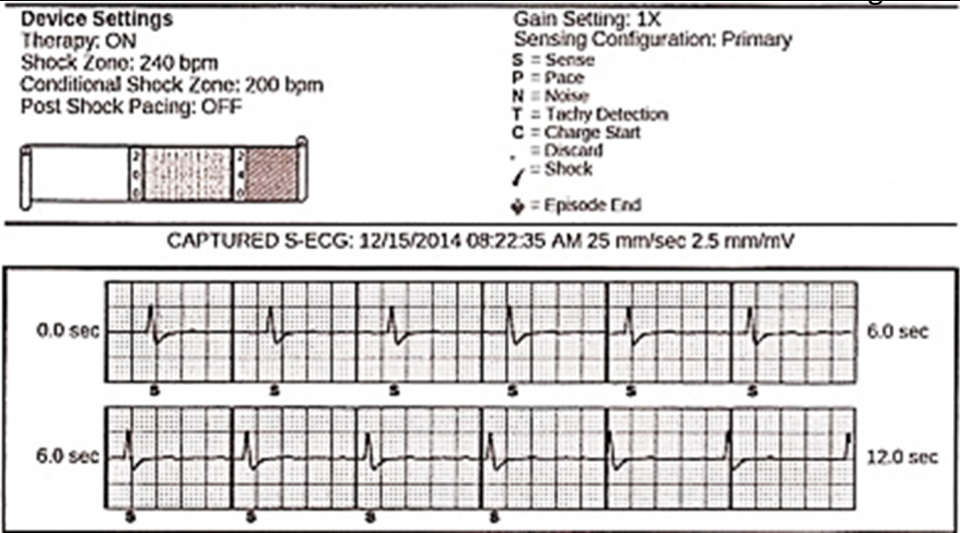
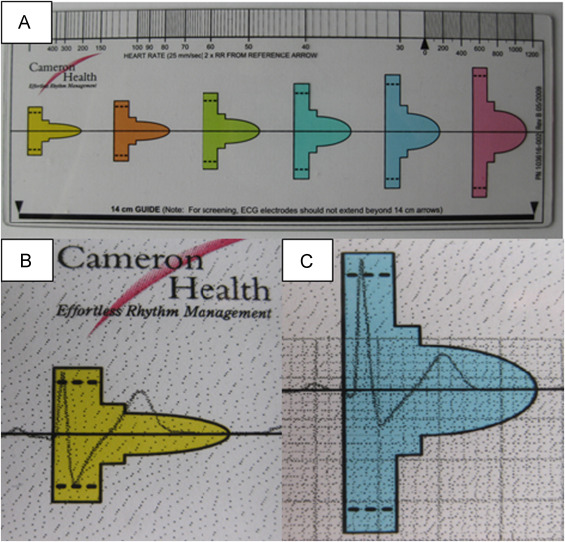
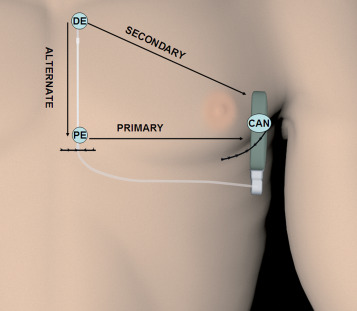
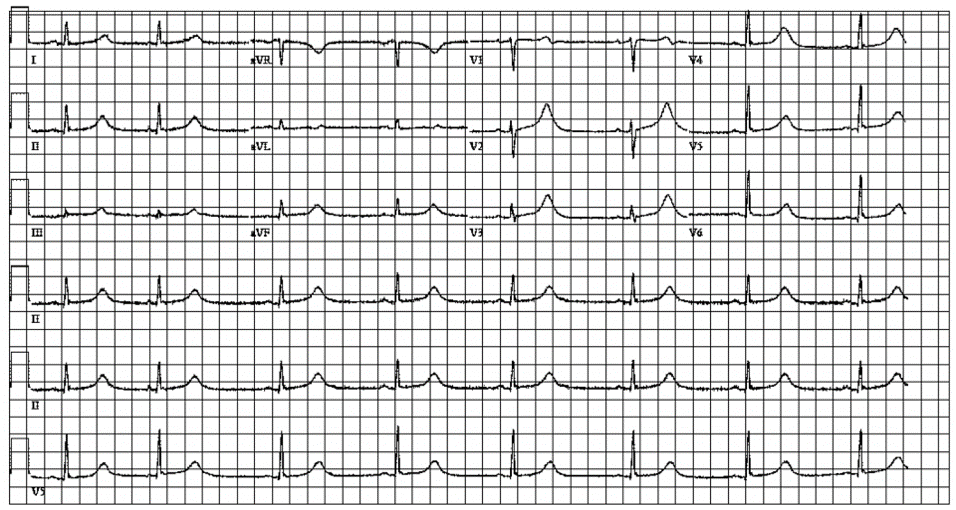
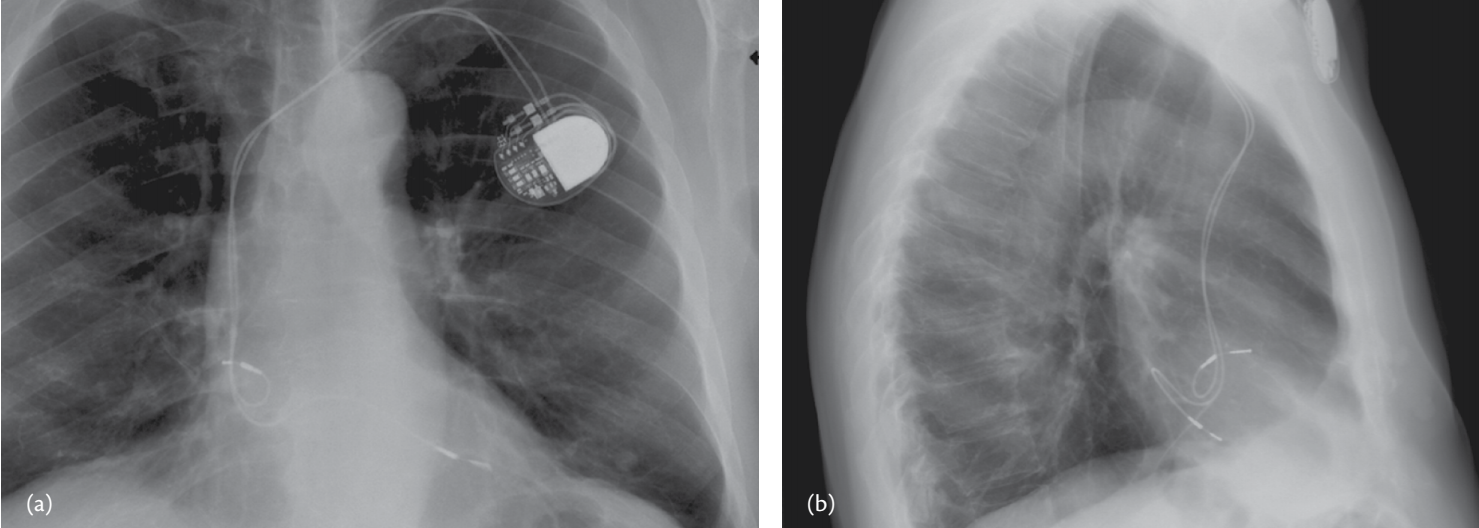
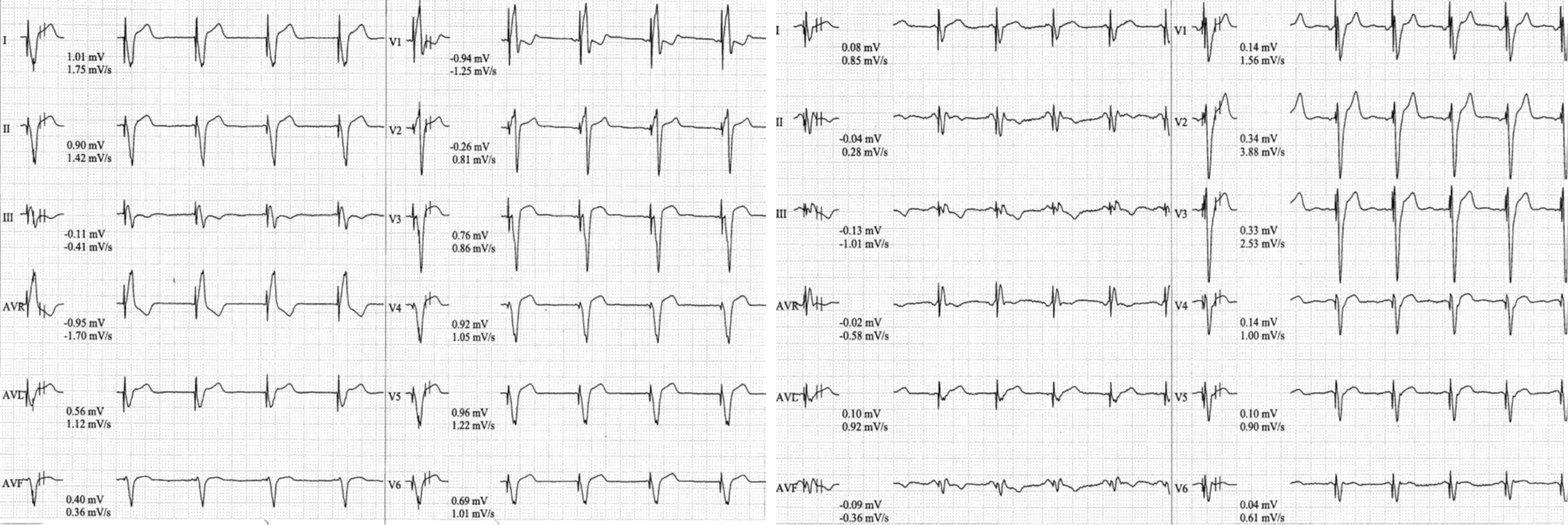 You are consulted to see a non-CRT responder. An exercise treadmill test
was performed. The tracings are as shown. What would be the most likely
cause of not responding to the CRT?
You are consulted to see a non-CRT responder. An exercise treadmill test
was performed. The tracings are as shown. What would be the most likely
cause of not responding to the CRT?

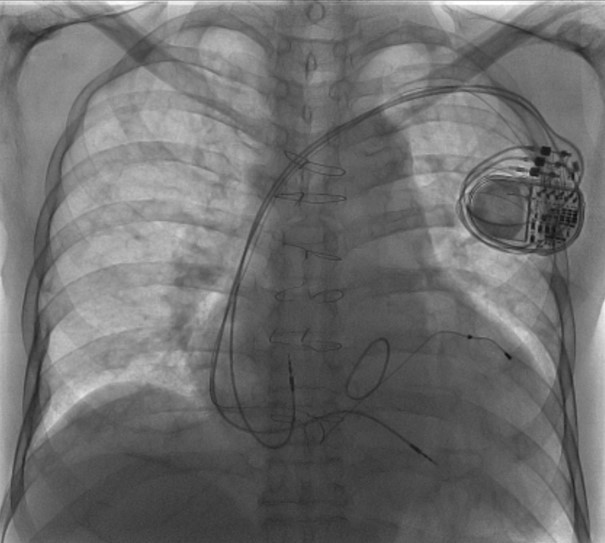
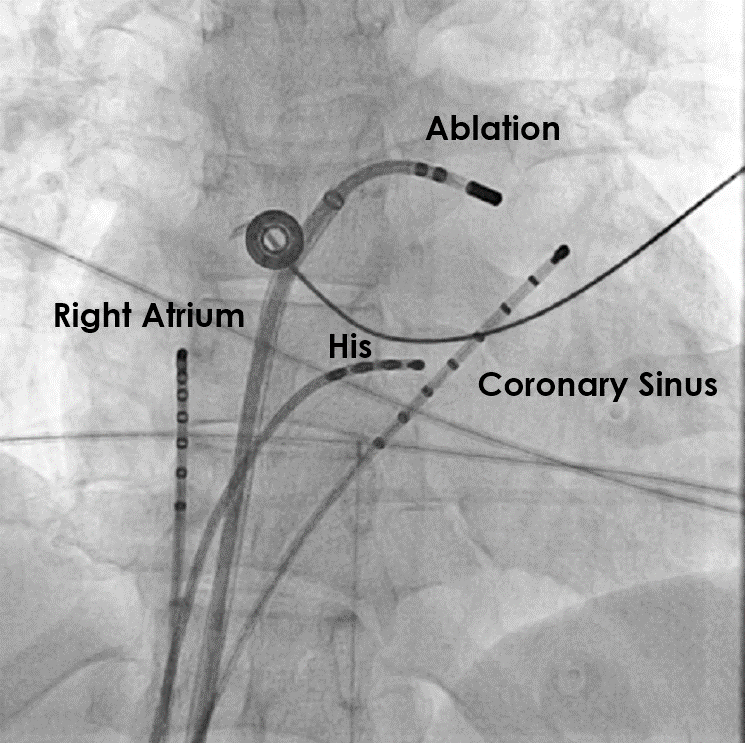
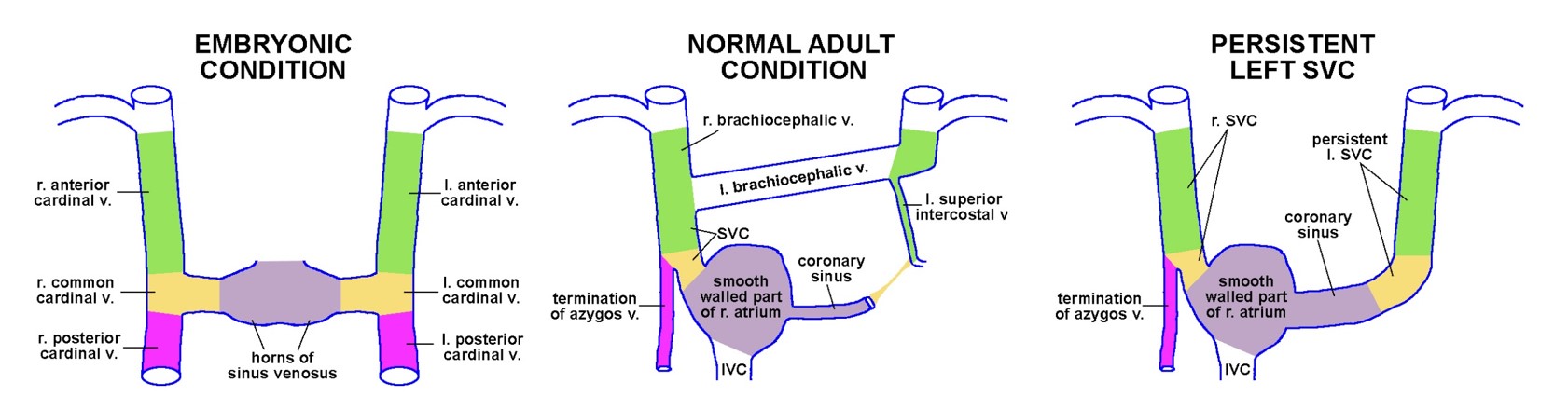 Persistent Left Superior Vena Cava is the most common variation of the thoracic venous
system. It is generally benign if found isolated.
Persistent Left Superior Vena Cava is the most common variation of the thoracic venous
system. It is generally benign if found isolated.