Our Collection
Our Collection
 Our Collection
Our Collection
 Show Answer
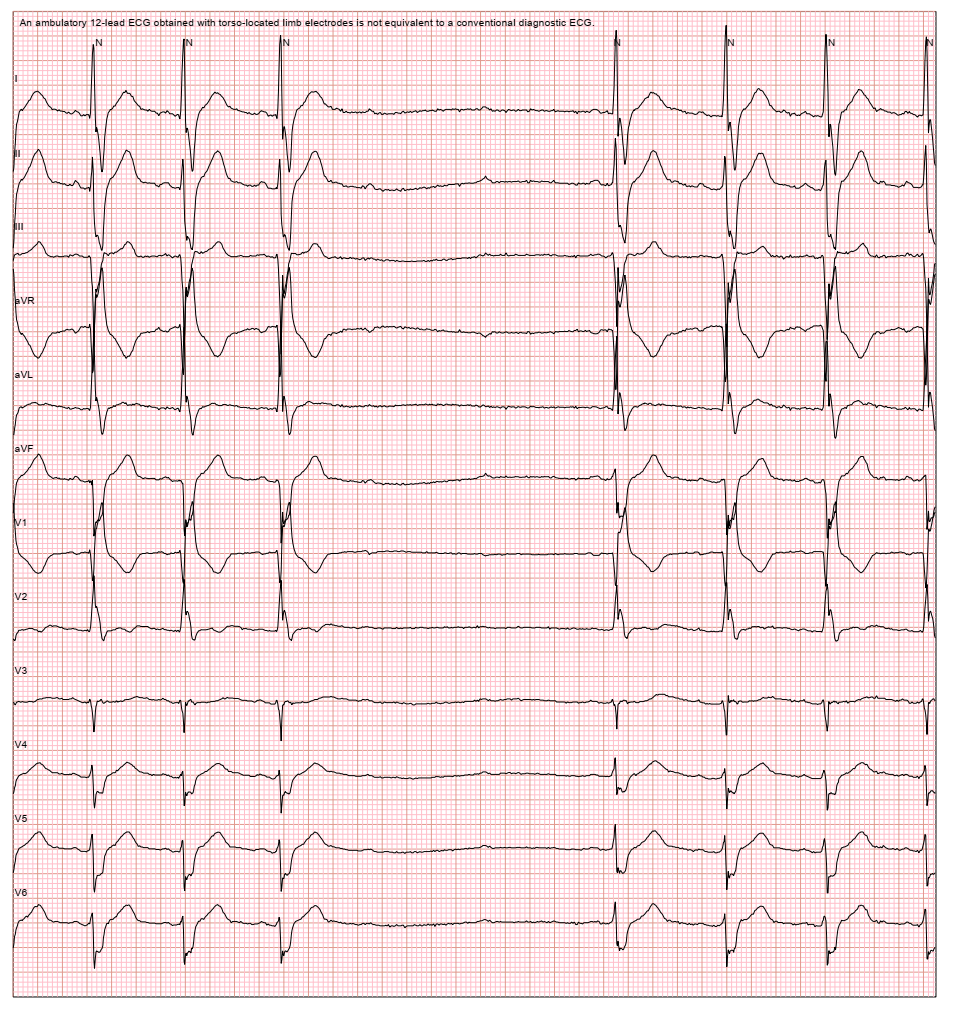
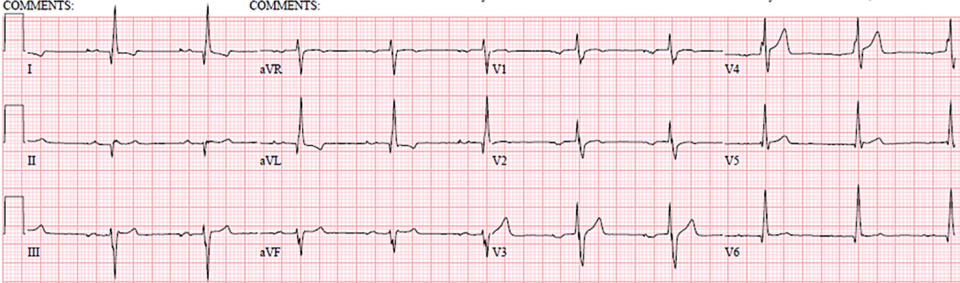
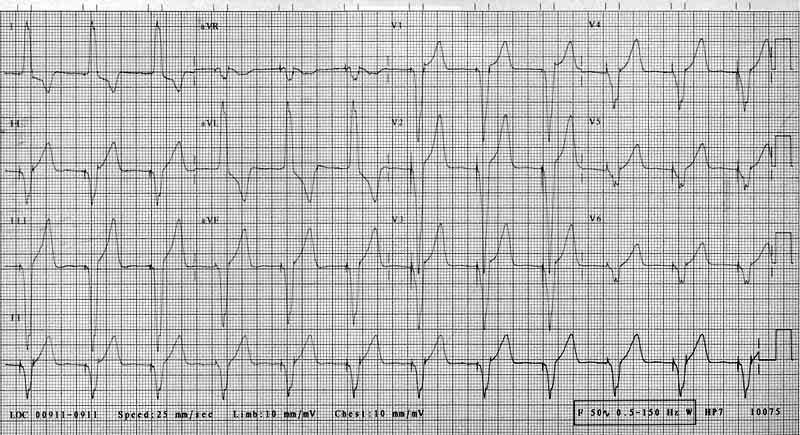
1st degree AV block. In a severe case (PR>330ms), symptoms similar to pacemaker syndrome
may occur.
Show Answer
1st degree AV block. In a severe case (PR>330ms), symptoms similar to pacemaker syndrome
may occur.
 Show Answer
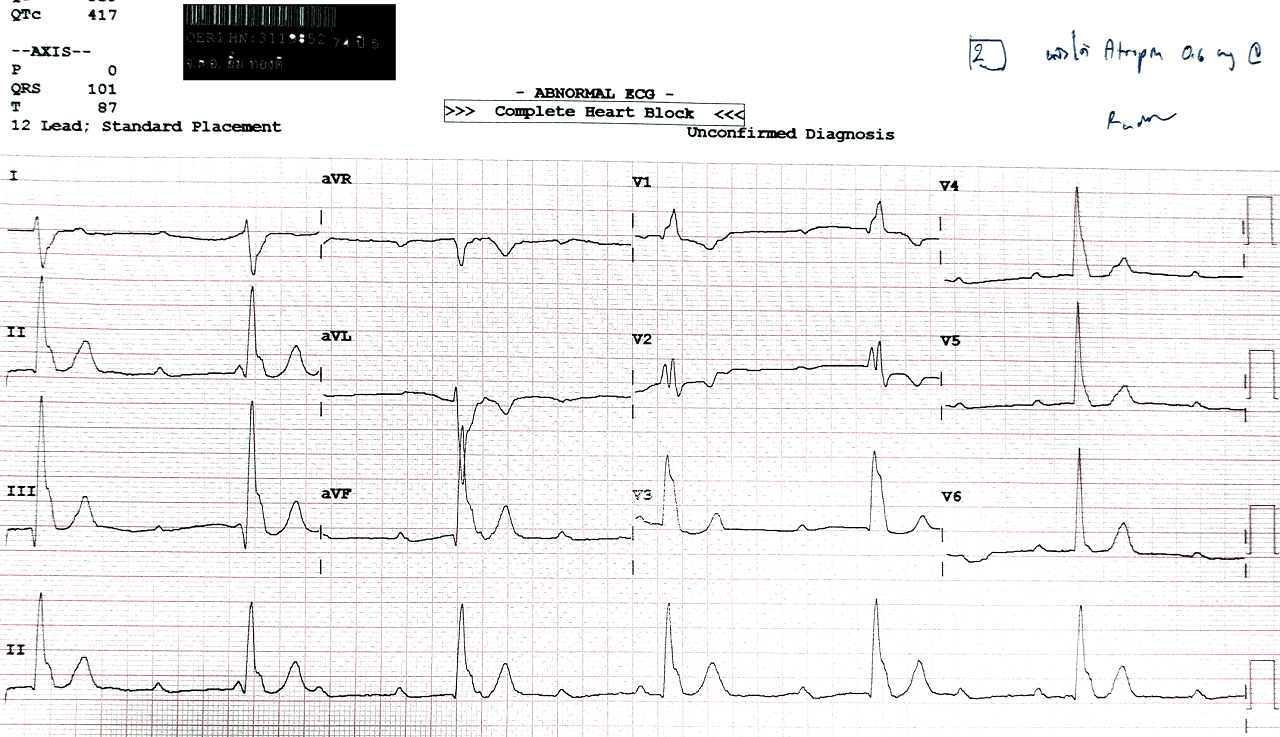
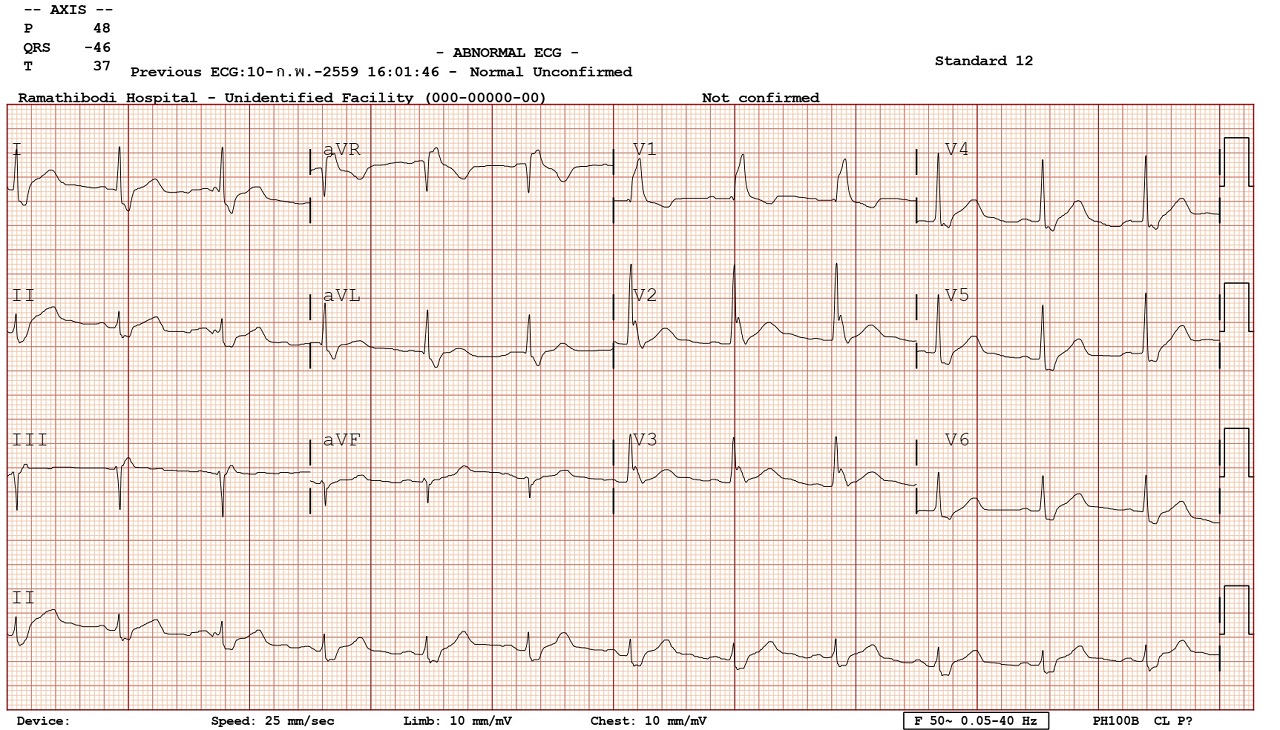
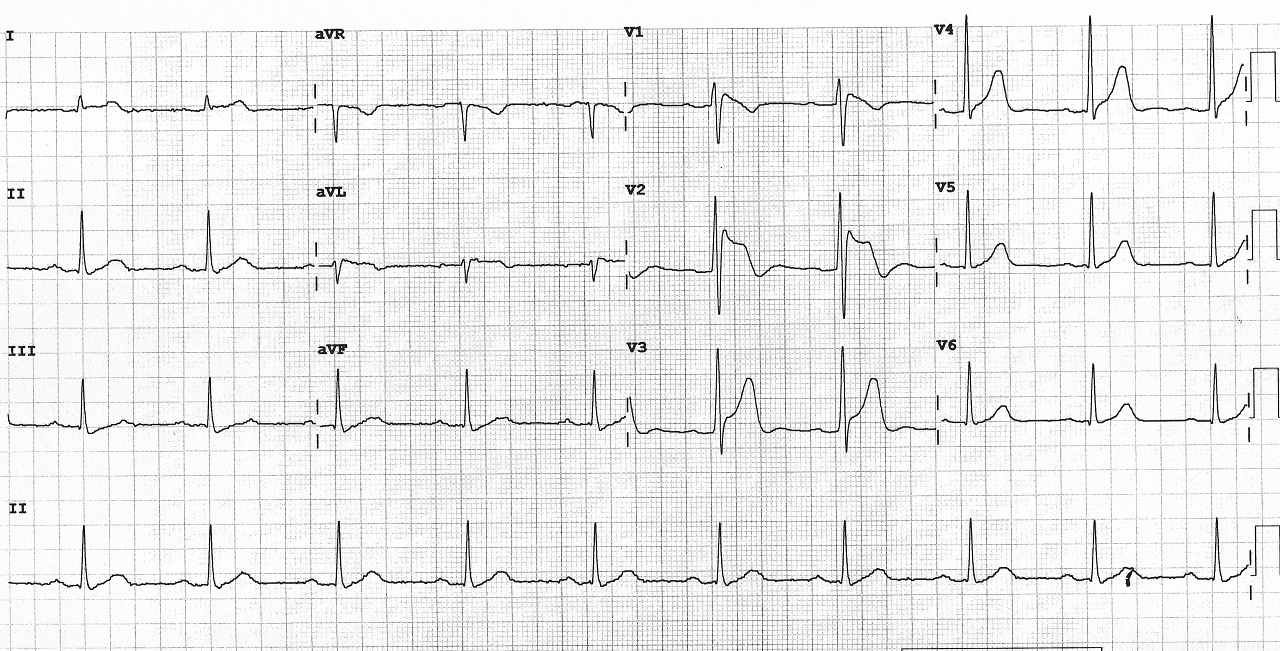
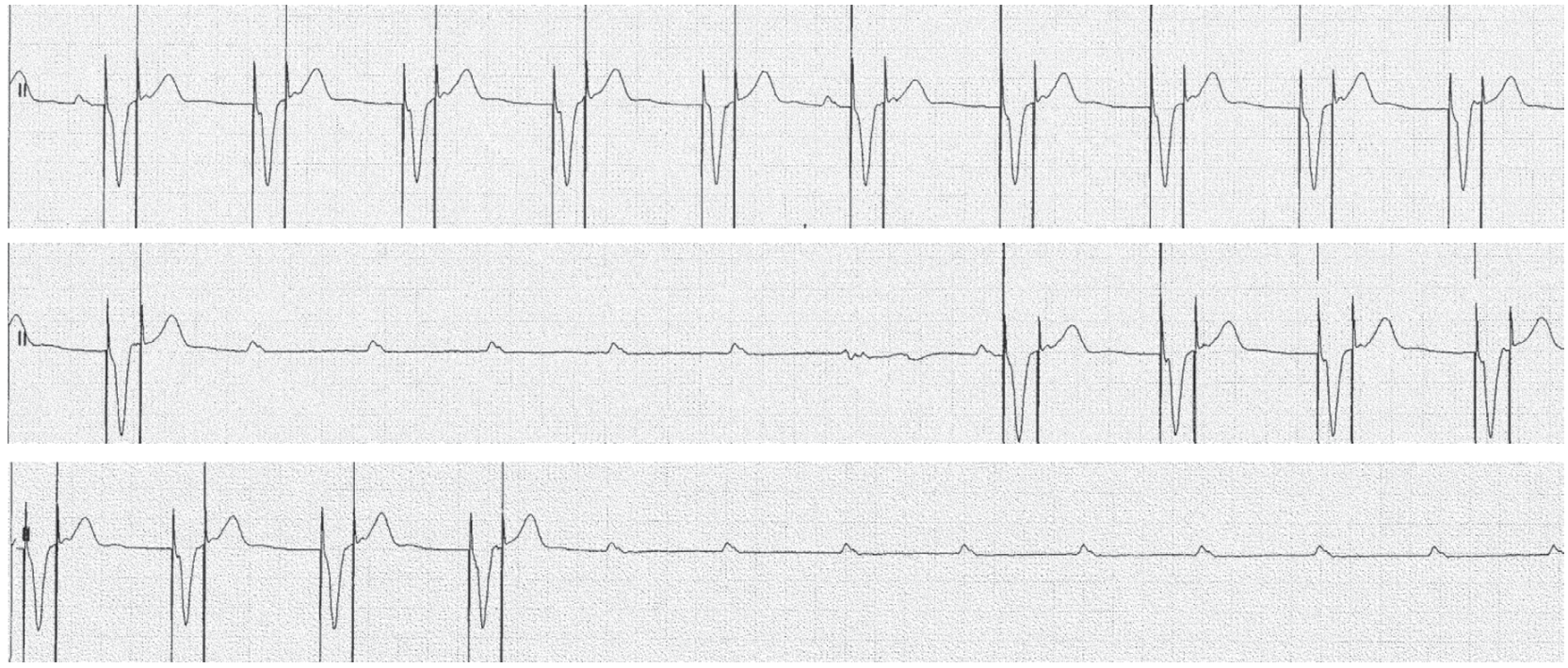
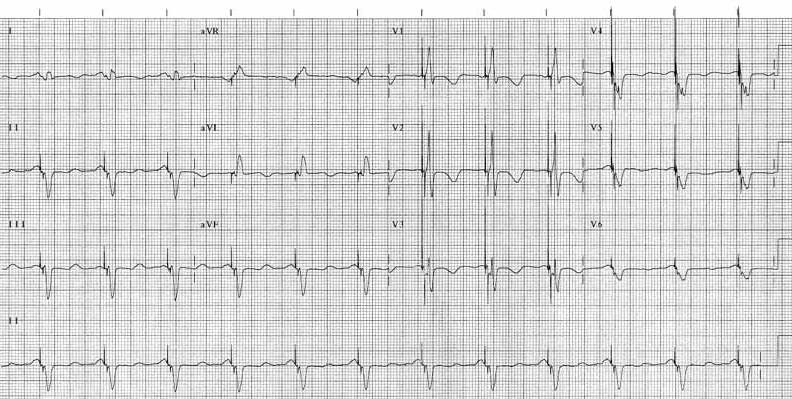
Intermittent complete heart block. 2Ps without any QRS. Underlying
rhythm is sinus rhythm with RBBB and LAFB.
Show Answer
Intermittent complete heart block. 2Ps without any QRS. Underlying
rhythm is sinus rhythm with RBBB and LAFB.
 Show Answer
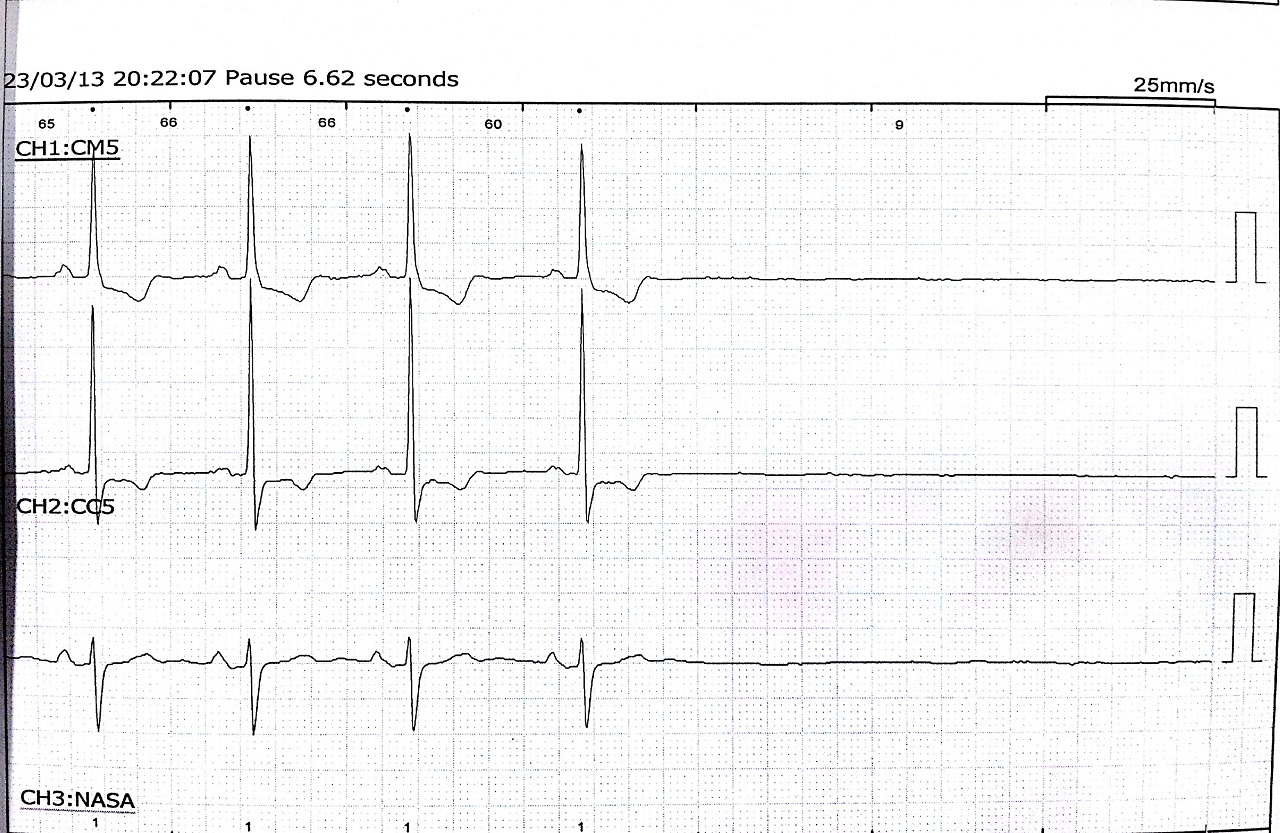
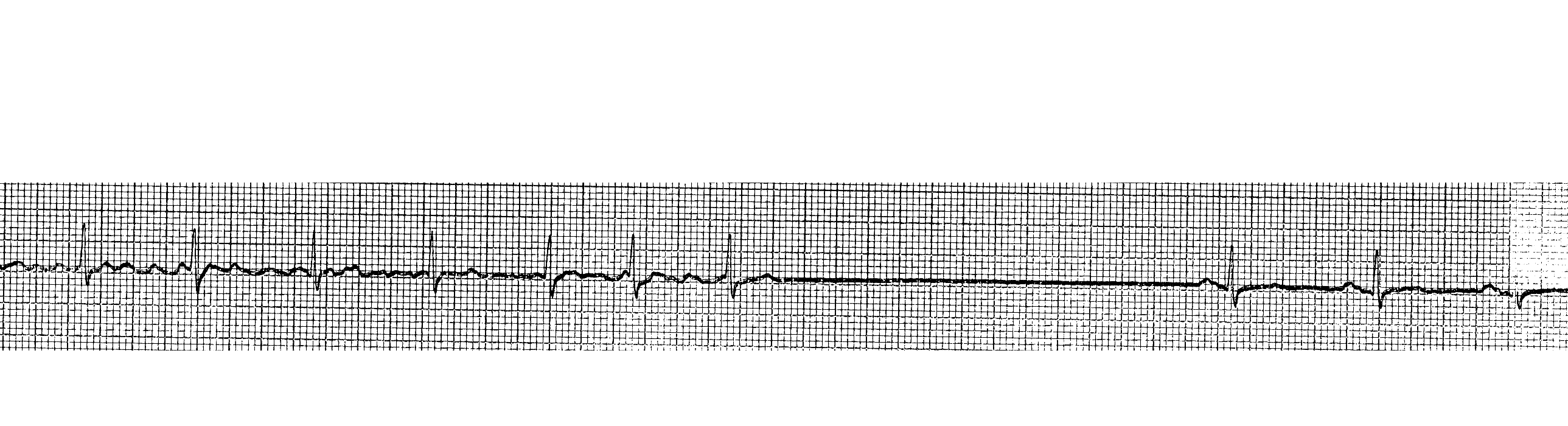
Sinus pause
Show Answer
Sinus pause
 Show Answer
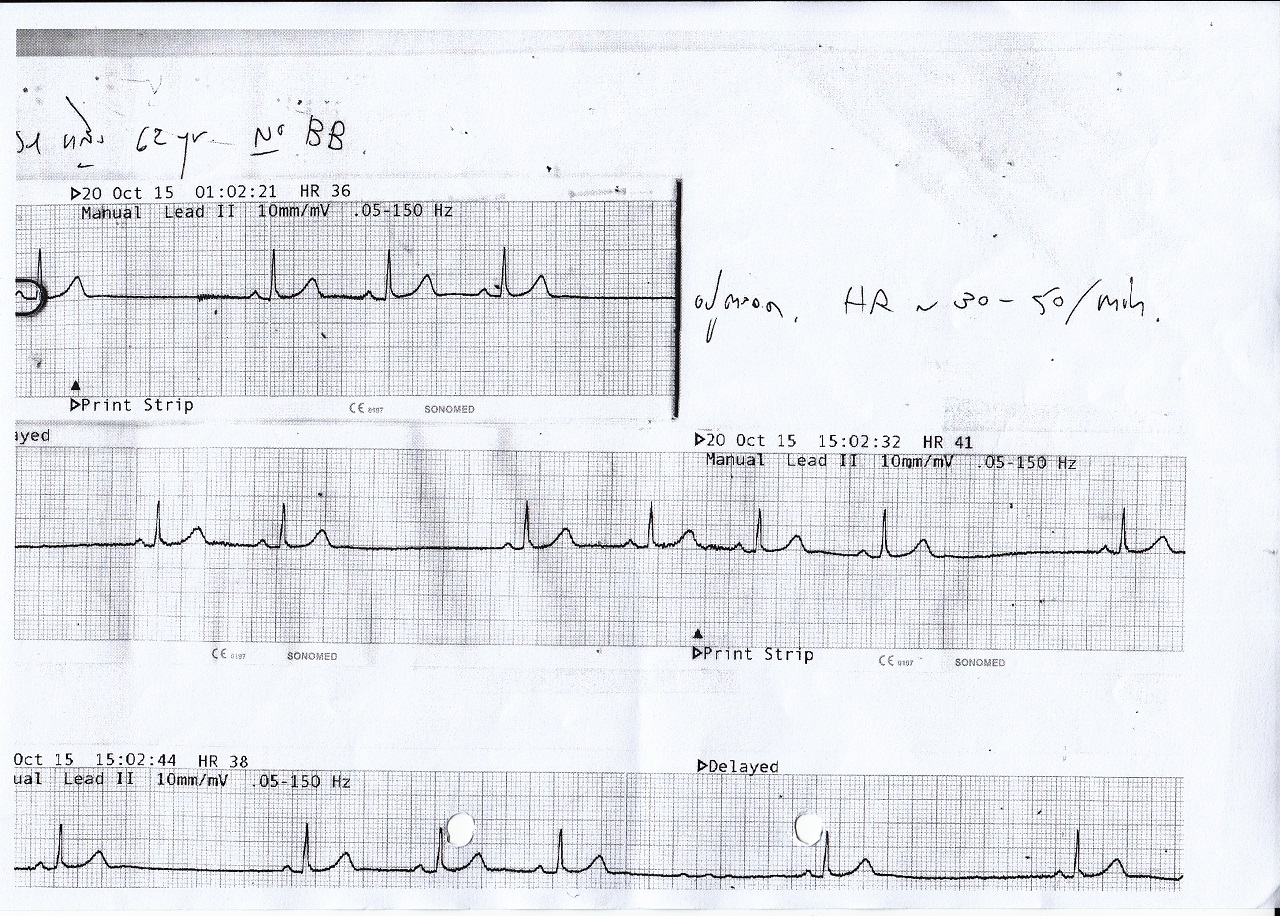
AF with conversion pause
Show Answer
AF with conversion pause
 Show Answer
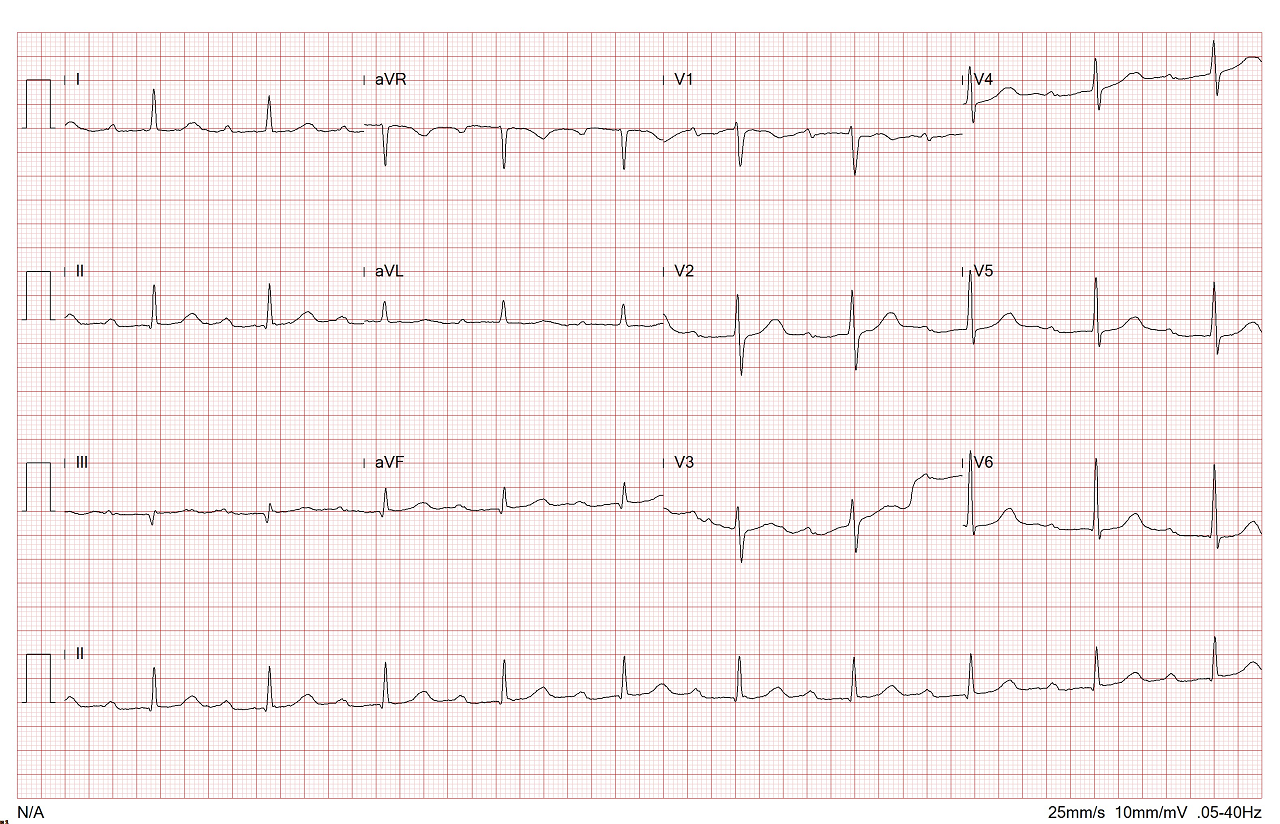
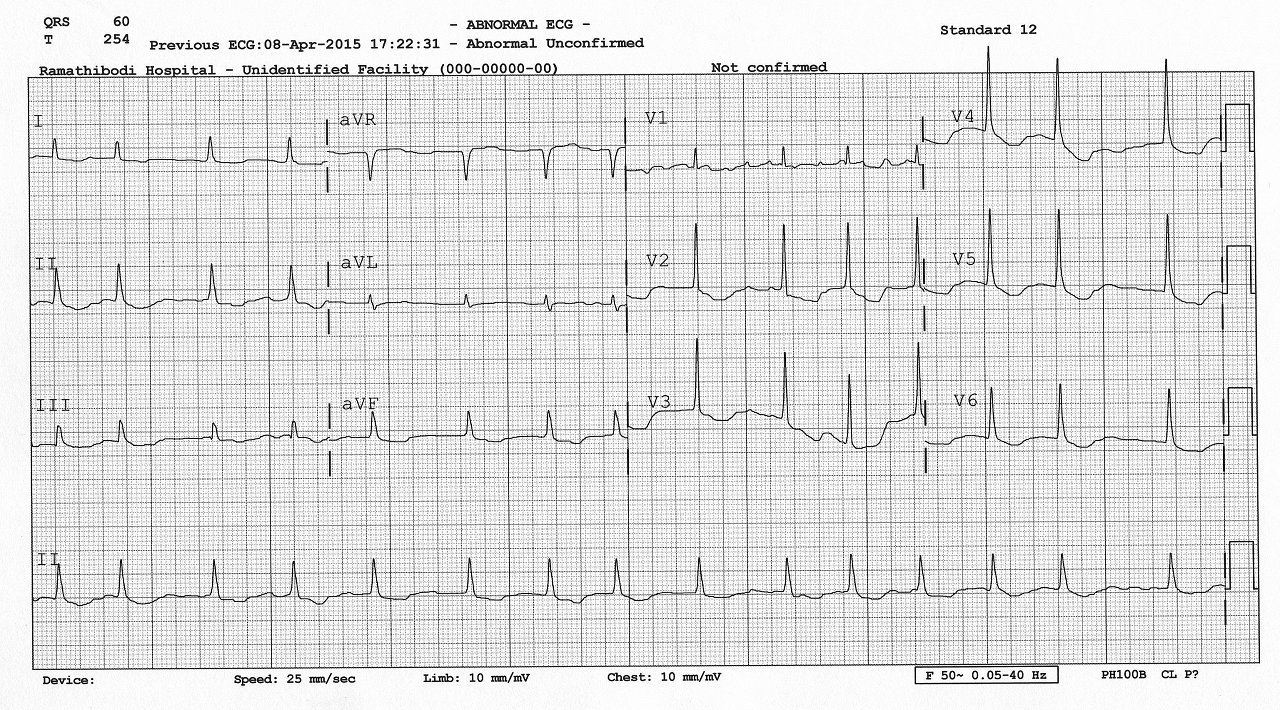
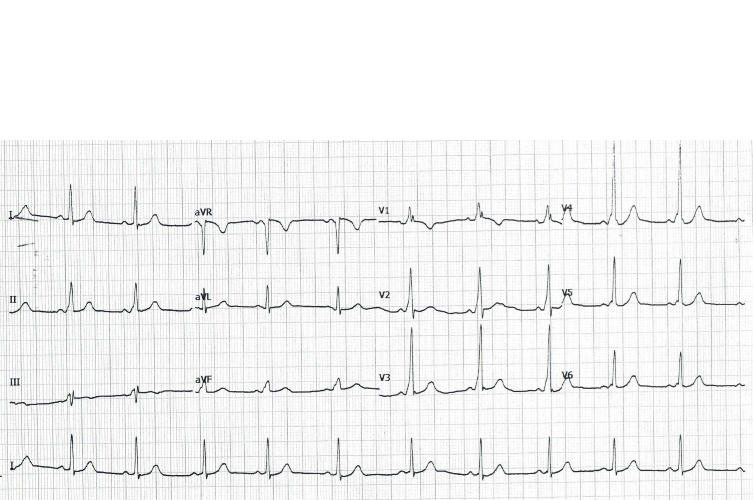
Atrial Fibrillation: irregularly irregular rhythm. Noted with fibrillatory waves in V1.
Show Answer
Atrial Fibrillation: irregularly irregular rhythm. Noted with fibrillatory waves in V1.
 Show Answer
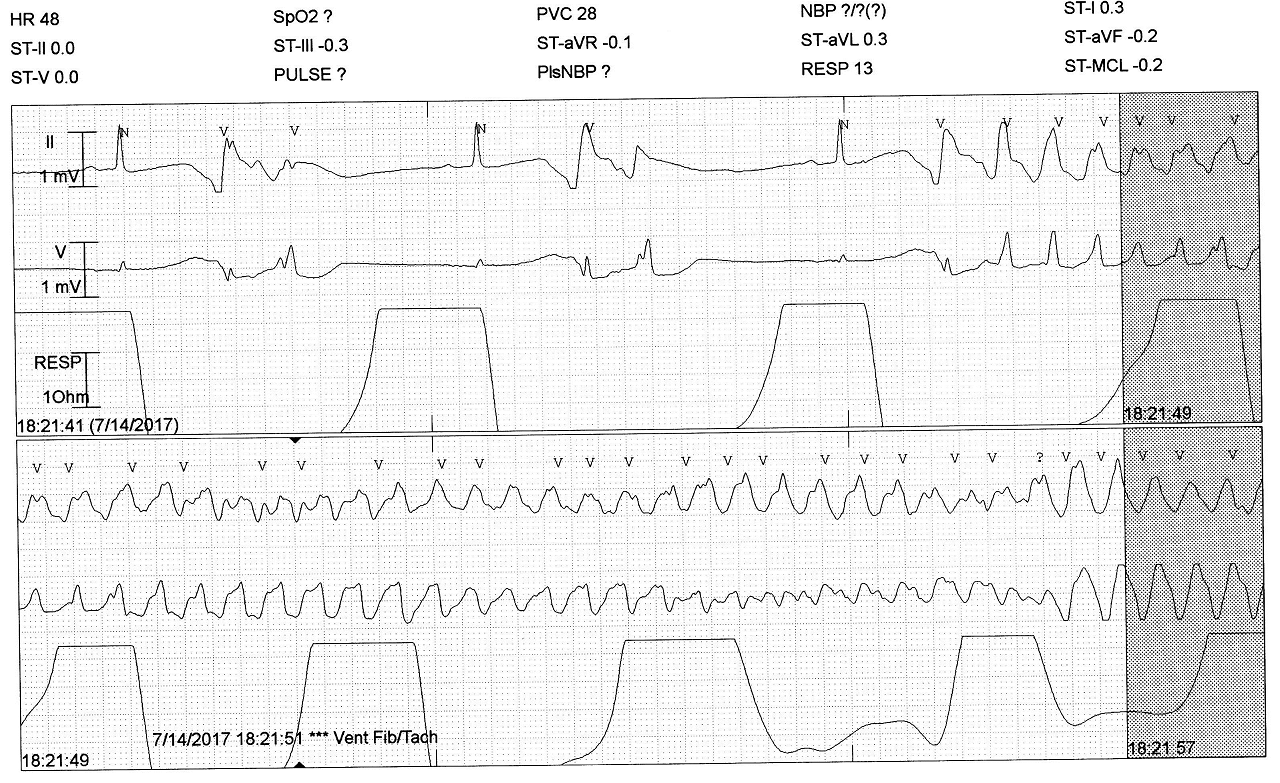
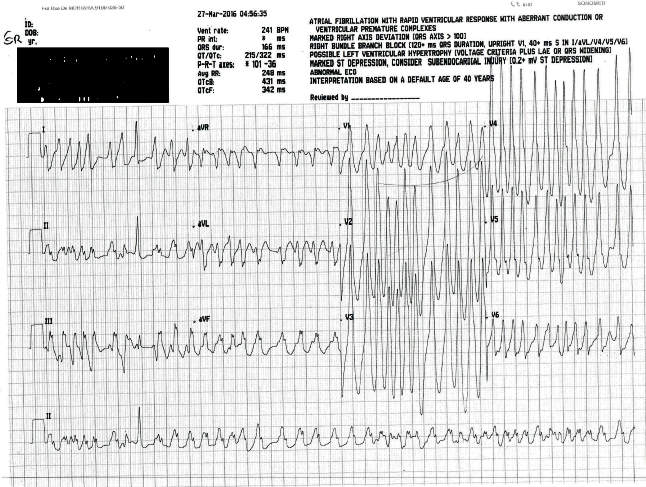
Polymorphic VT with long QT or Torsade de Pointes.
Show Answer
Polymorphic VT with long QT or Torsade de Pointes.
 Show Answer
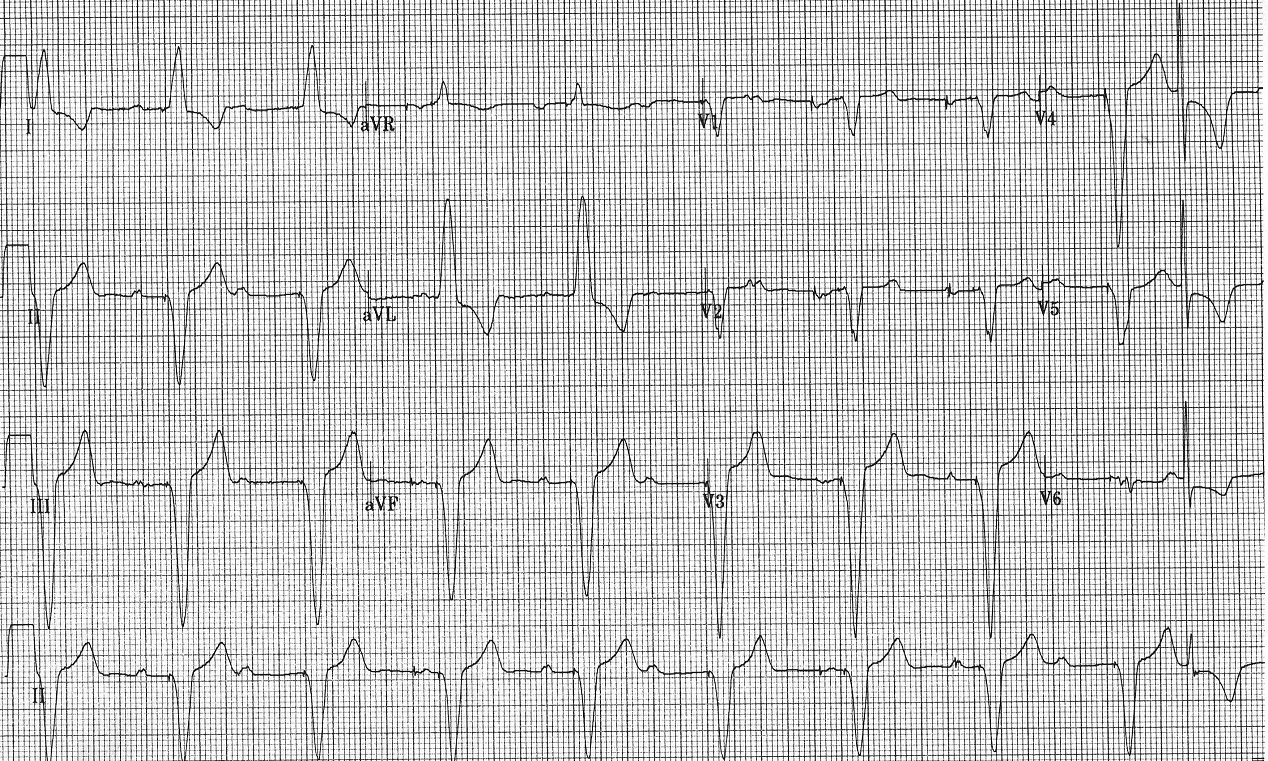
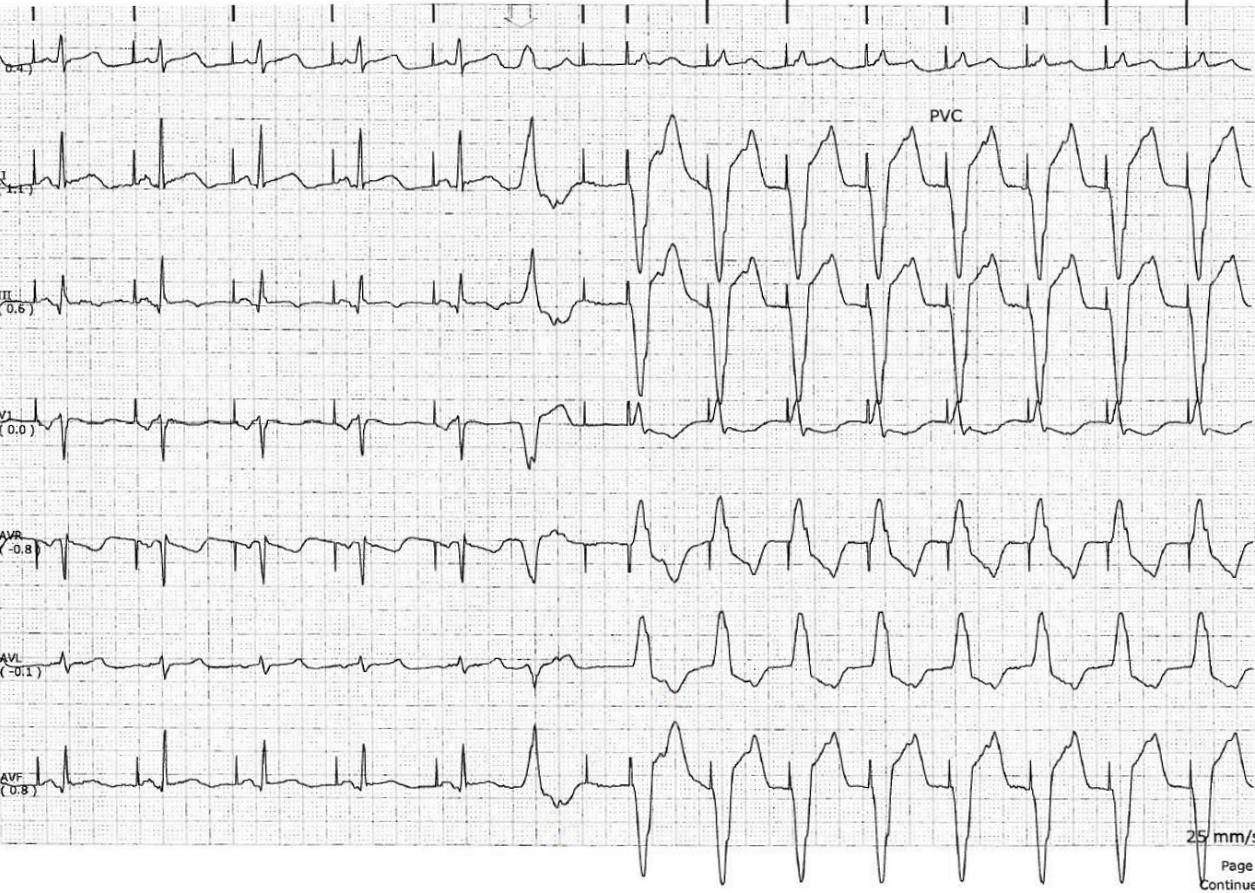
Ischemic VT in a patient with history of inferior wall MI.
Show Answer
Ischemic VT in a patient with history of inferior wall MI.
 Show Answer
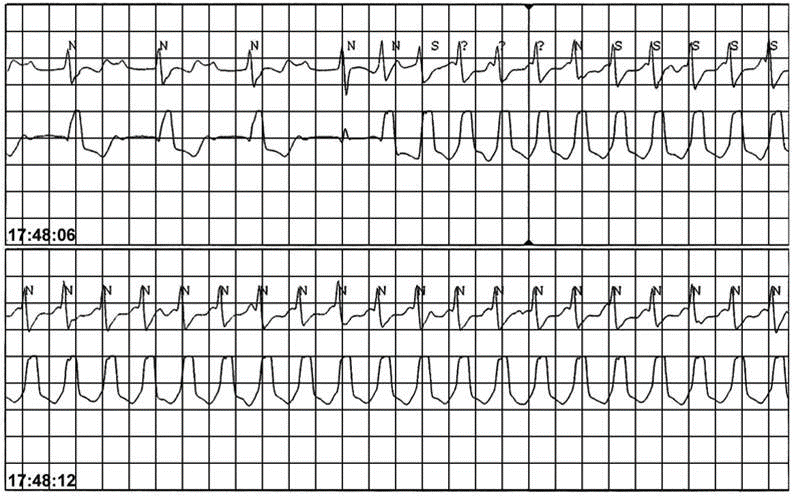
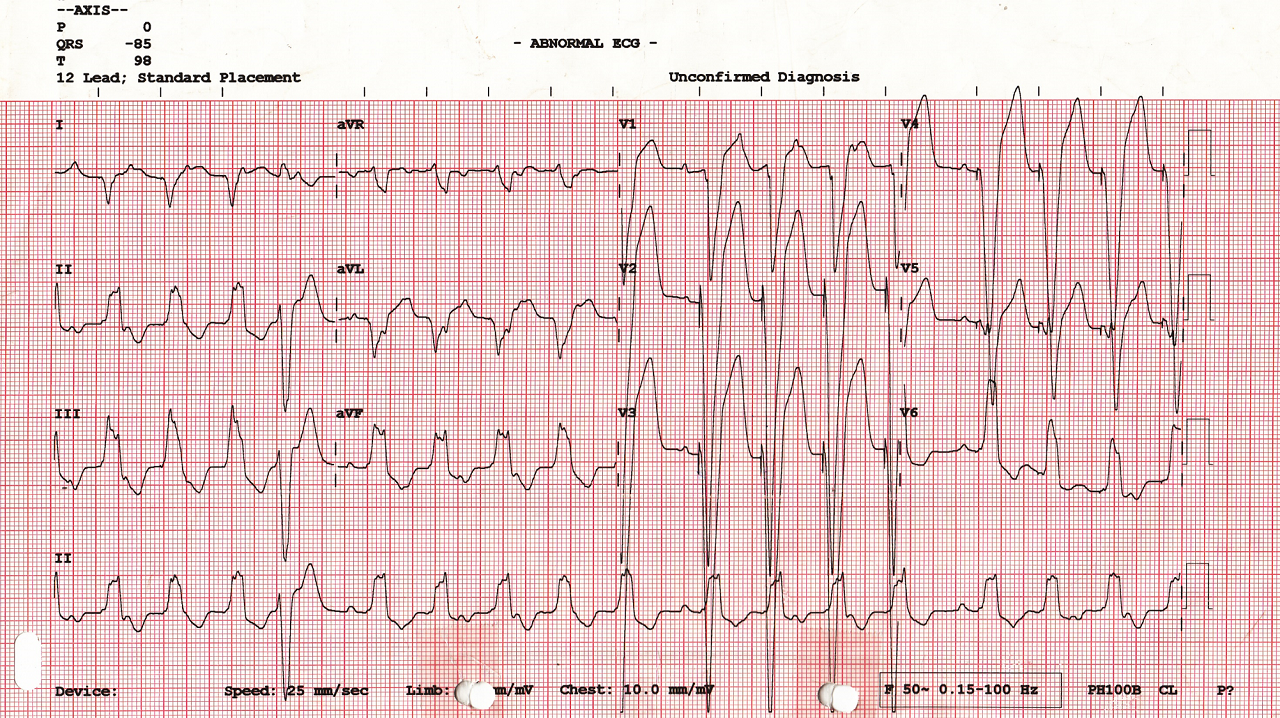
Monomorphic VT. VA dissociation is clearly seen.
Show Answer
Monomorphic VT. VA dissociation is clearly seen.
 Show Answer
Brugada ECG: J point elevation with coved-type ST elevation in V1-V2.
Show Answer
Brugada ECG: J point elevation with coved-type ST elevation in V1-V2.
 Show Answer
Hypertrophic cardiomyopathy: high voltage in left-sided leads with ST depression and
T wave inversion.
Show Answer
Hypertrophic cardiomyopathy: high voltage in left-sided leads with ST depression and
T wave inversion.
 Show Answer
Long QT
Show Answer
Long QT
 Show Answer
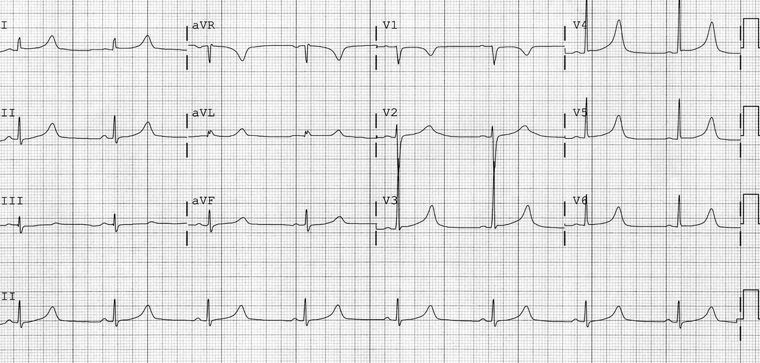
Old MI; Noted with Q waves in inferior and anterior leads.
Show Answer
Old MI; Noted with Q waves in inferior and anterior leads.
 Show Answer
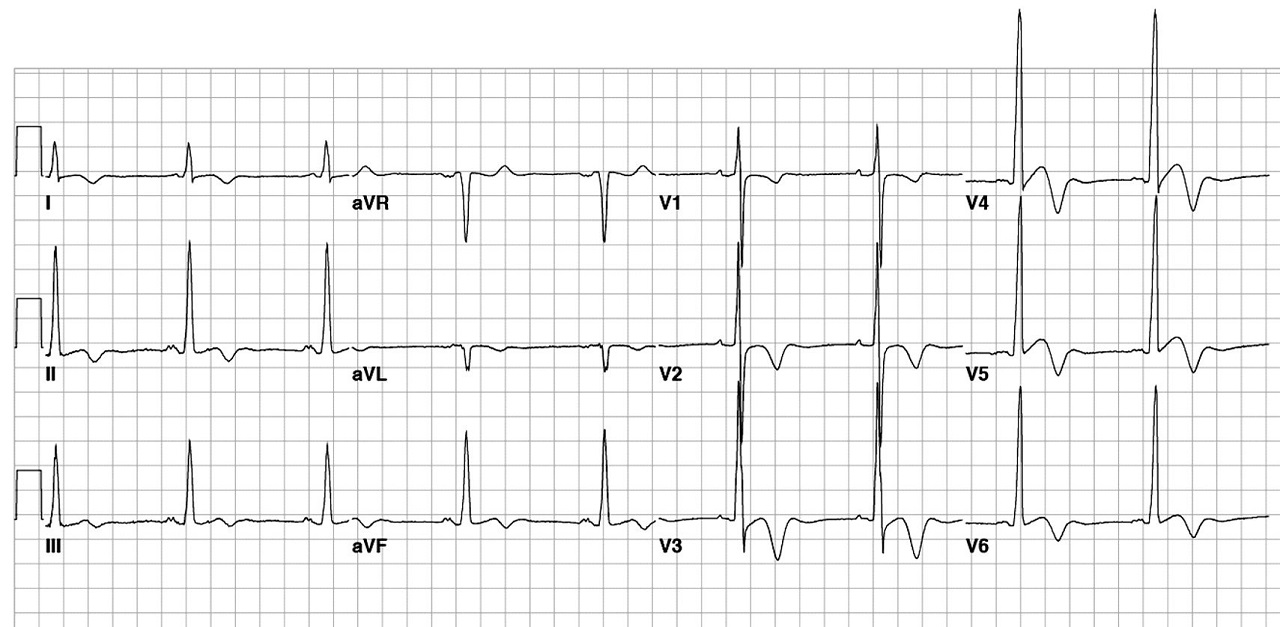
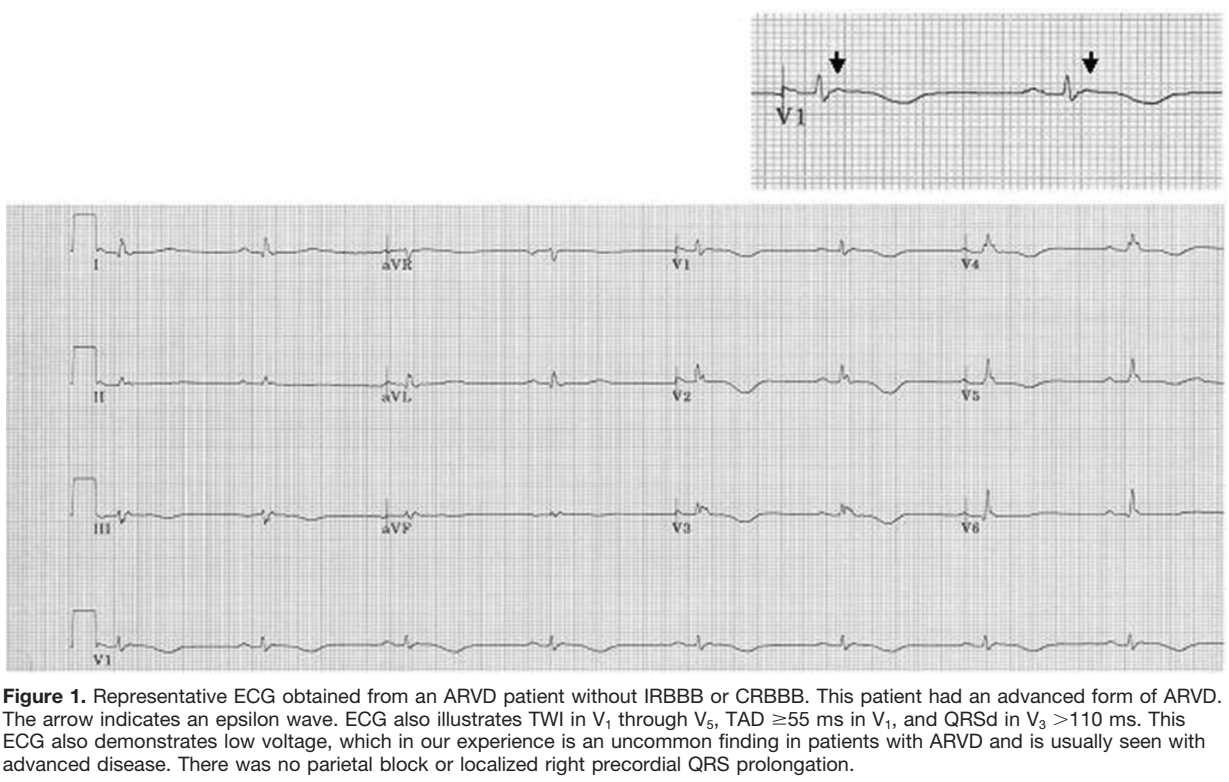
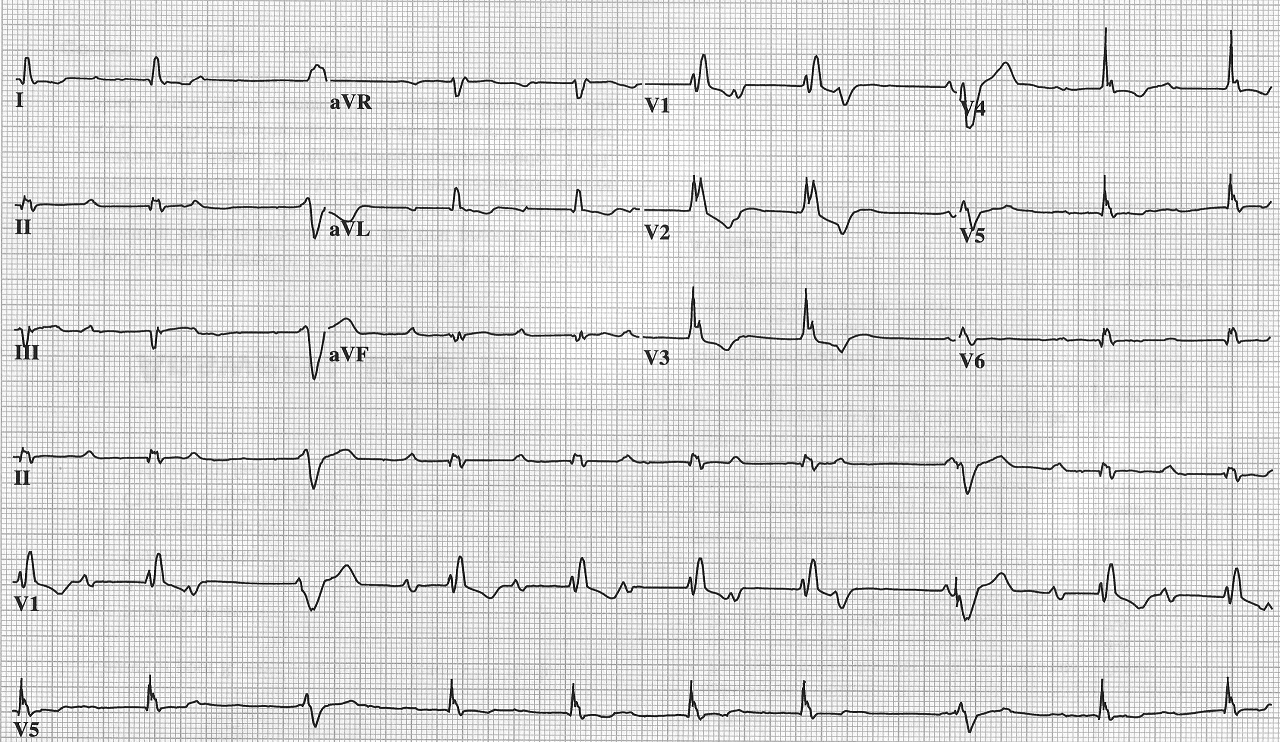
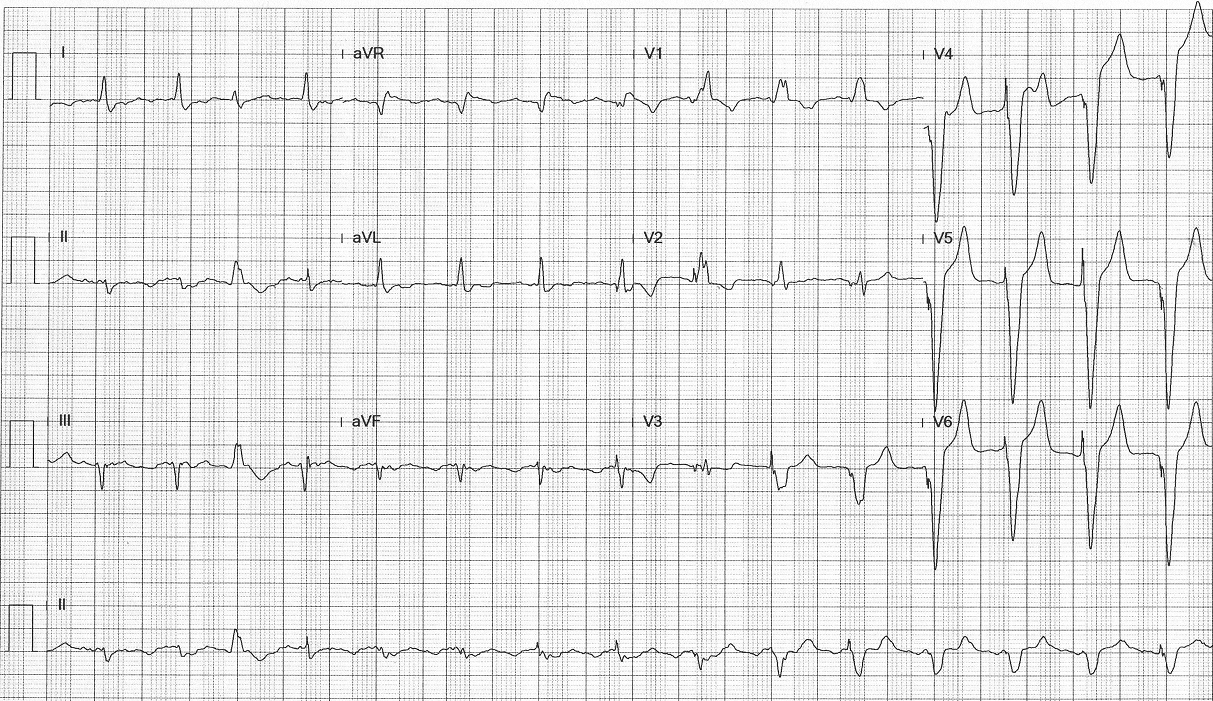
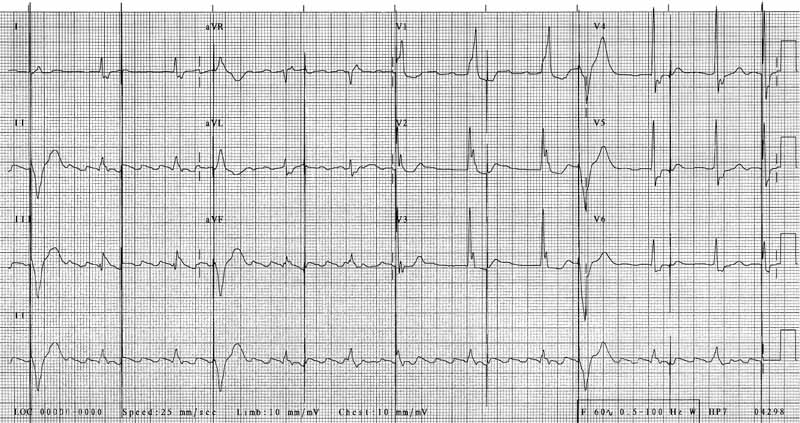
Arrhythmogenic right ventricular dysplasia (ARVD), a disease of right ventricule.
Characteristic ECG findings include Epsilon wave (delay in depolarization) and
T wave inversion in V1-V4.
Show Answer
Arrhythmogenic right ventricular dysplasia (ARVD), a disease of right ventricule.
Characteristic ECG findings include Epsilon wave (delay in depolarization) and
T wave inversion in V1-V4.
 Show Answer
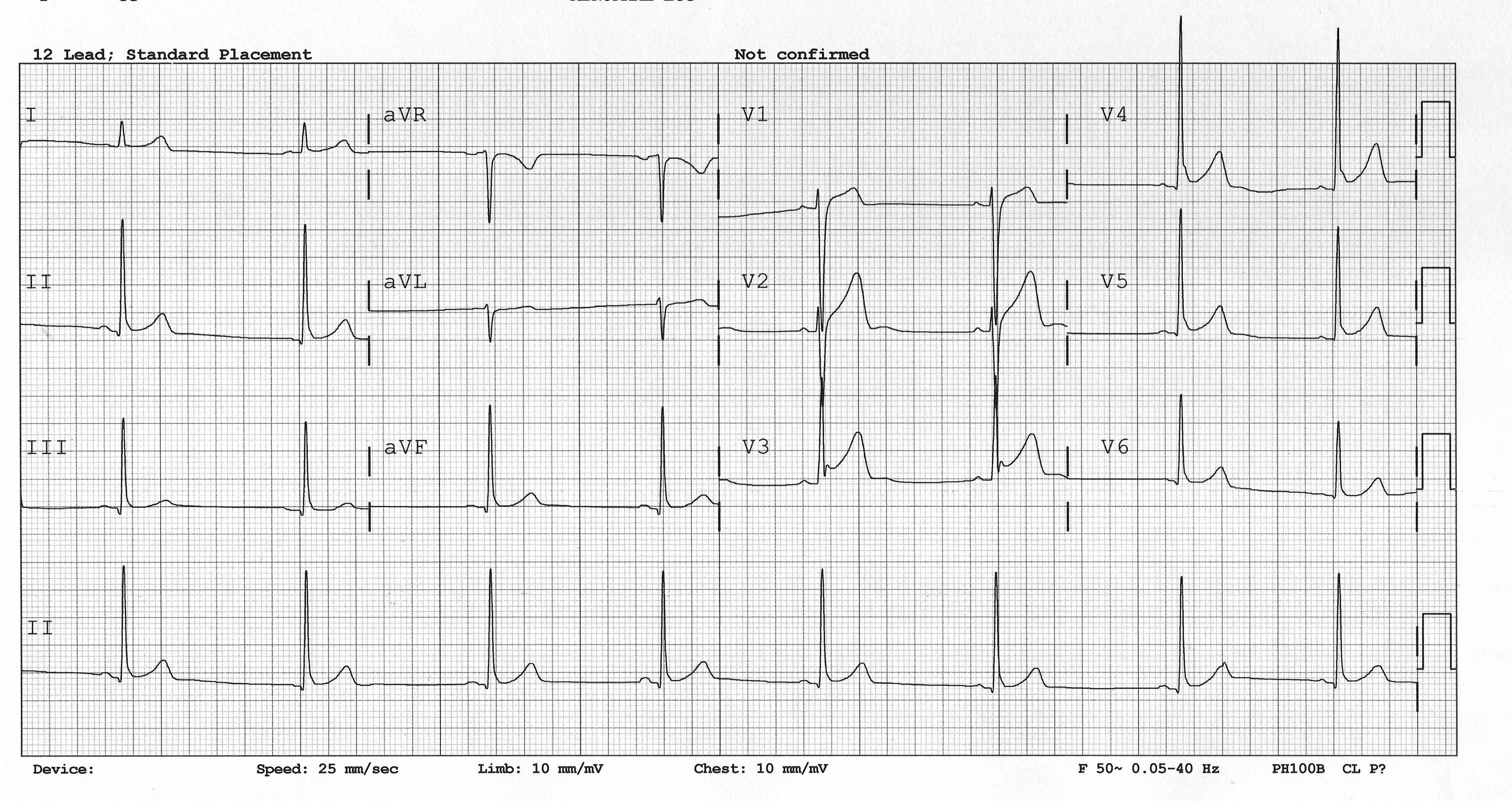
Early repolarization: J point elevation concaved downward ST elevation.
Show Answer
Early repolarization: J point elevation concaved downward ST elevation.
 Show Answer
Short QT
Show Answer
Short QT
 Show Answer
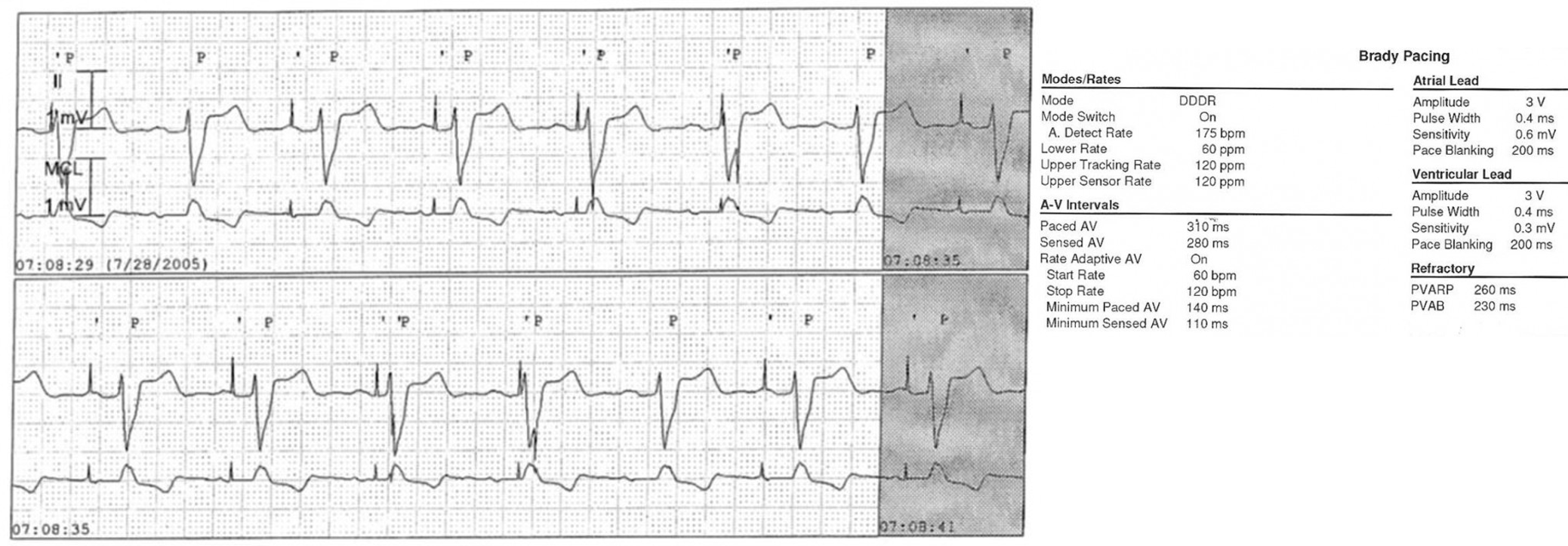
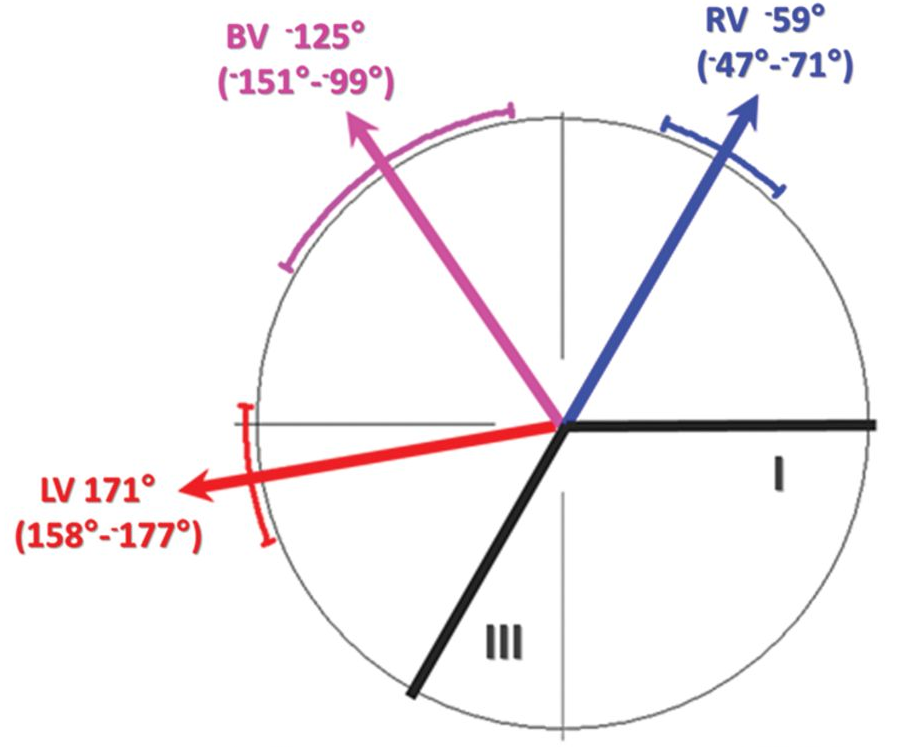
A and V leads switch in the header. Ventricular pacing is being inhibited by P wave (middle tracing),
ruling out lead dislodgement (there needs to be a lead in atrium).
Inhibition of V pacing is intermittent due to higher sensitivity in A channel.
Show Answer
A and V leads switch in the header. Ventricular pacing is being inhibited by P wave (middle tracing),
ruling out lead dislodgement (there needs to be a lead in atrium).
Inhibition of V pacing is intermittent due to higher sensitivity in A channel.
 Show Answer
Normal pacemaker function. DDI 60, AVD 200.
Show Answer
Normal pacemaker function. DDI 60, AVD 200.
 Show Answer
Normal pacemaker function. Rhythm = sinus rhythm with AV Wenckebach.
V pacing came on the dropped beats.
Show Answer
Normal pacemaker function. Rhythm = sinus rhythm with AV Wenckebach.
V pacing came on the dropped beats.
 Show Answer
Pacemaker mediated tachycardia; triggered by a PVC with retrograde P, followed
by an non-capture A pacing with long AV delay, allowing the following retrograde
VA conduction to capture the atrium and initiate PMT.
Show Answer
Pacemaker mediated tachycardia; triggered by a PVC with retrograde P, followed
by an non-capture A pacing with long AV delay, allowing the following retrograde
VA conduction to capture the atrium and initiate PMT.
 Show Answer
Sinus tachycardia with pacemaker Wenckebach.
Show Answer
Sinus tachycardia with pacemaker Wenckebach.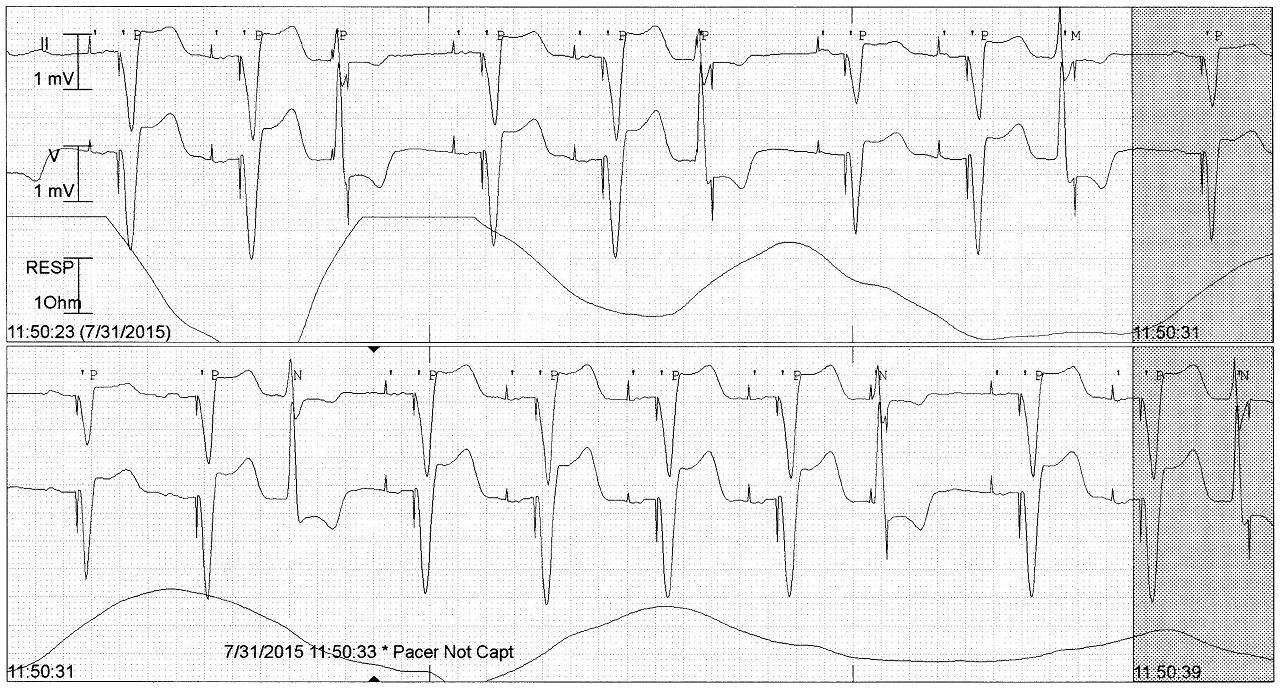 Show Answer
Safety pacing triggered by timely PVCs. Noted with short AV delays.
Show Answer
Safety pacing triggered by timely PVCs. Noted with short AV delays.
 Show Answer
Managed ventricular pacing: AAI mode switches to DDD with short AV delay after
AP without native ventricular beat.
Show Answer
Managed ventricular pacing: AAI mode switches to DDD with short AV delay after
AP without native ventricular beat.
 Show Answer
Sinus tachycardia above upper rate limit; hence no biventricular pacing.
Show Answer
Sinus tachycardia above upper rate limit; hence no biventricular pacing.
 Show Answer
The atrial lead has dislodged into the ventricle. Ventricular captures are seen
by the first spike (from atrial lead) followed by a functional non-capture from the second spike (from
ventricular lead).
Show Answer
The atrial lead has dislodged into the ventricle. Ventricular captures are seen
by the first spike (from atrial lead) followed by a functional non-capture from the second spike (from
ventricular lead).
 Show Answer
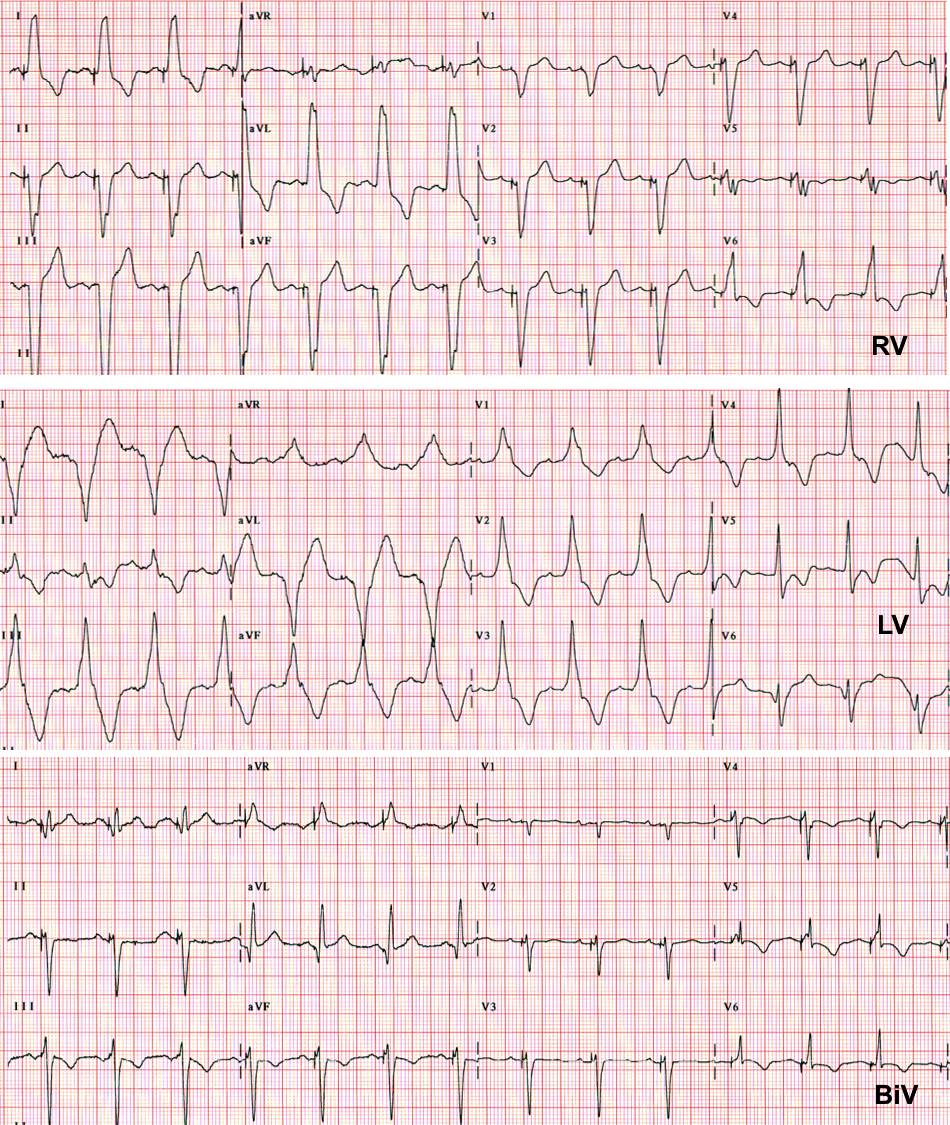
Normal CRT function with VV delay of 40ms.
Show Answer
Normal CRT function with VV delay of 40ms.
 Show Answer
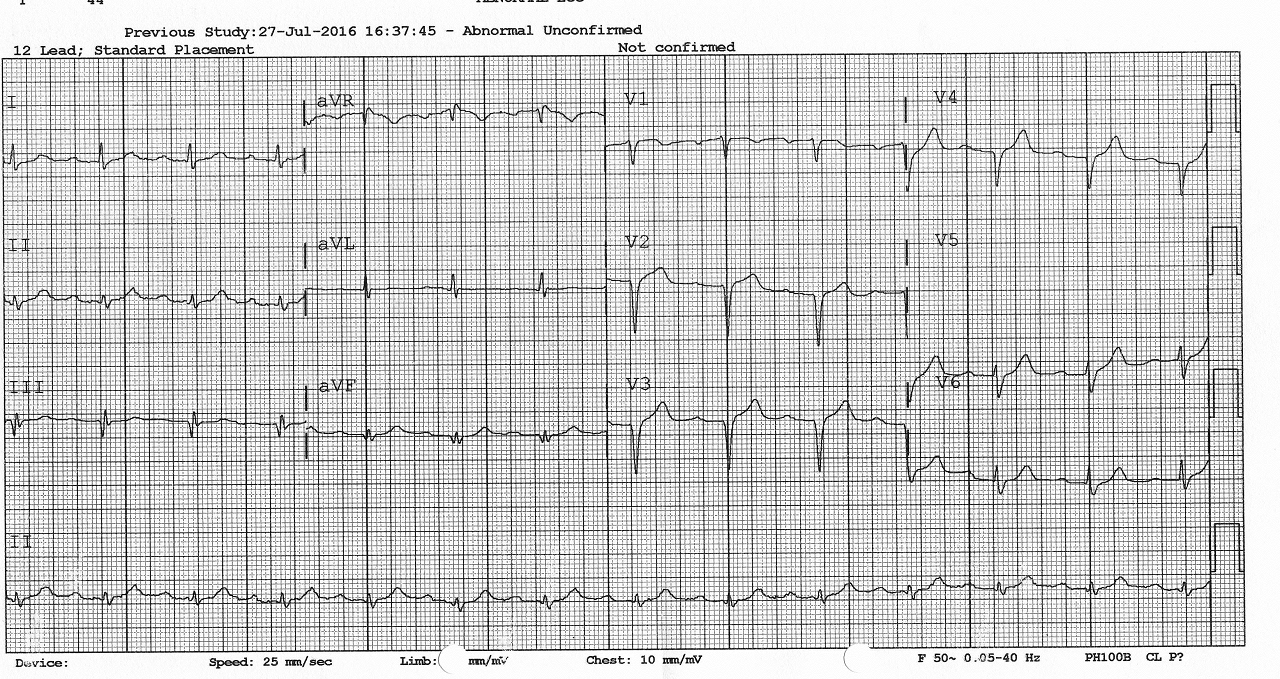
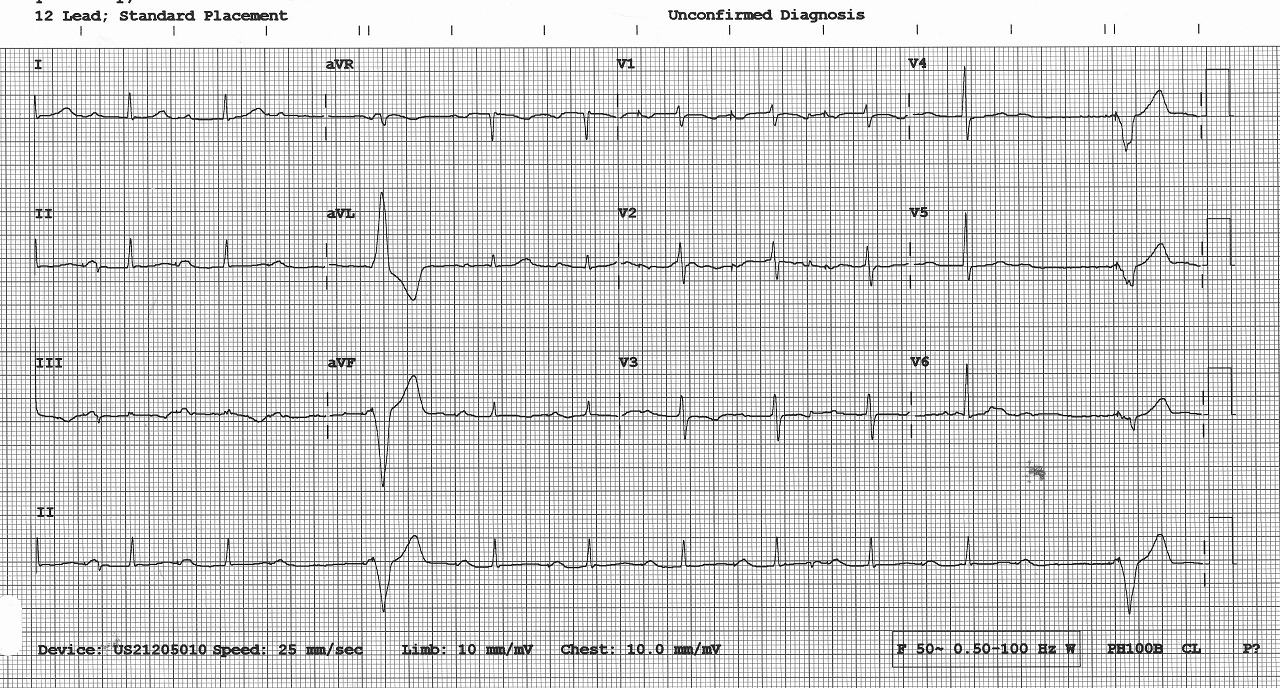
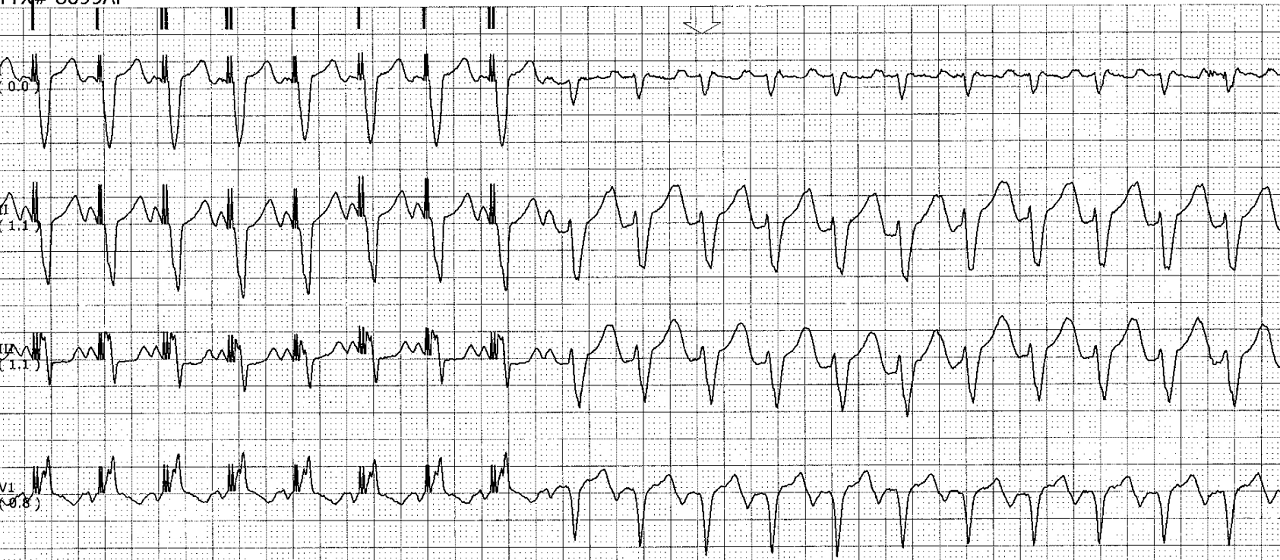
Pacemaker failure. Radiation may cause deterioration of lead and pacemaker
circuit. ECG show asynchronous pacing. Urgent generator change is needed.
Show Answer
Pacemaker failure. Radiation may cause deterioration of lead and pacemaker
circuit. ECG show asynchronous pacing. Urgent generator change is needed.